A Budding Emergencist
Wednesday, August 30, 2006
Ahh, farewell ER (for now)
Ok, the stone has turned. My last ER shift has come and gone. It was a make-up shift, and it actually overlapped my Anaesthesia rotation by one day, so I missed orientation (wah.) Now I am in Anaesthesia (I prefer the English spelling), and generally enjoying it. My anaesthesia attending says that it is more important to know your anesthesiologist's credentials and understand what's involved in that aspect of a case as opposed to the surgeon, but after watching a CT surgeon do (surgere? surgerize?) a 6-hr, off-pump CABG on a 81-years-young patient, I'm not so sure. Both are important, I expect.
Seeing Sid Schwab and Scalpel as well as "old pal" platypus comment on my blog is nice. Thanks!
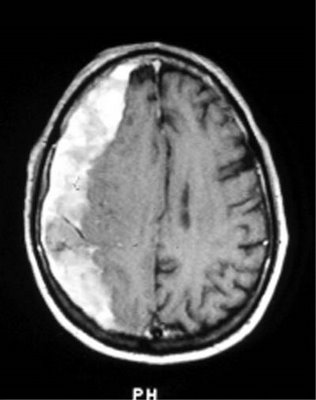
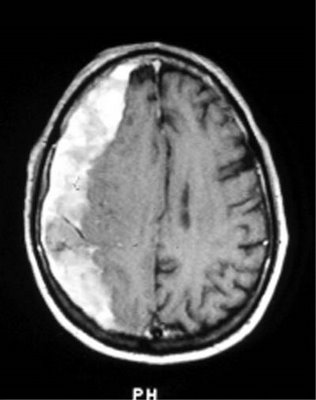
We had another VIP today at Metropolitan Medical Center, coming in for a 2 month old subacute subdural hematoma--a little out of the range (3 weeks) for subacute vs chronic, but that walked and talked like a subacute. Story goes, she (director of nursing for psychiatry, a nice lady and I trust her) was involved in a bad car wreck 2 months back, with her husband unfortunately receiving some pretty nasty lower extremity fractures. She got a nasty bump on her head along with some nausea/vomiting, and after the CT was read as normal, she was diagnosed with postconcussion syndrome. In the intervening two months, while her husband was being worked up for his fractures, she supported him while quietly cataloging and circular-filing her own symptoms, which included transient recurrent minor weakness in her left leg, transient numbness/tingling in her left arm, and an intruiging strip of paresthesia starting from the lateral canthus of her right eye and extending laterally into her scalp, not associated with tearing or dry eye. No N/V since then, no syncope, no cardiopulmonary symptoms, no seizures, no decreased level of consciousness.
[intermission: while these findings constitute focal neurologic signs, thus excluding PCS, I can imagine how, even in an experienced nurse, such a "diagnosis" can lead someone to minimize their symptoms until they become an impairment--"Oh, it's just my PCS acting up".]
[intermission #2: Nurses give great histories! This was like taking report on a patient instead of grinding out a history. VIP's are nice, for this and more reasons--they speak English, know their meds, know their history, and aren't afraid of mentioning things that other people would think the doctor "didn't need to know," like that bad reaction they had to penicillin 30 years ago resulting in an ICU stay, because medicine has really progressed since then, right?]
[there is NO intermission #3]
Being that the patient's regular doc was on vacation, she worked her grapevine to get expedited through the ER via my-favorite-attending, stopping by the CT and MRI machines for what she believed to be a transient ischemic attack, or mini-stroke. Well, she ended up fast-tracked to neurosurgery, where I saw her.
After a good deal of hand-patting, visits from our innumerable VP's and anxious relatives (uh, I mean, cowworker nurses), and a closed-session pep-talk by my anaestheia attending (who says anaesthesiologists don't talk to patients?), we got underway. After we had intubated and got some lines started, we waited around for the neurosurgeon awhile (sigh.). Finally the neurosurgery physician assistant comes in and immediately starts yelling! at my senior attending, for current and previous imagined slights! Agog, I stare unbelieving at this joker while he rants and whines about my attending for imagined slights (she wanted to talk to the surgeon about the case instead of this flunky) and finally leaves in a drama-queen huff. I mean, what is up with neurosurg PA's? They all seem to have a chip on their shoulder the size of Manhattan.
After the (rather young, given the 8-year residency neurosurgeon had come in and received his dose of abuse from the PA (while I again am shocked, chagrined, and stupefied at his impertinence. In the OR!), the surgery began. Nicely routine, with an interesting sidenote of how a subacute subdural will form a membrane around itself, leading to reformation of the hematoma despite every effort to prevent it. The surgeon explained that there is no way to prevent this, because stripping this extra membrane actually leads to increased recurrence of subdurals, and there is no way to "make the brain expand", like you would for a chronic pulmonary effusion to prevent recurrence. Long story short, the neurosurgeon started with Burr holes to evacuate the hematoma, and finding mainly solid hematoma, had to take out a chunk of skull to evacuate it, but otherwise the procedure went well, about 3 hours from the first cut.
After a teeth-grinding wait for transportation, I went and found a monitor myself after repeated overhead calls for a monitor (apparently VIP status doesn't faze the nursing attendants, of whom I've heard tell that if they stand up too fast they pass out. Trust an ER doc to do it himself. After that, our VIP went to recovery in the surgical intensive care unit, safe in the capable and caring hands of our SICU nurses.
Ok, the stone has turned. My last ER shift has come and gone. It was a make-up shift, and it actually overlapped my Anaesthesia rotation by one day, so I missed orientation (wah.) Now I am in Anaesthesia (I prefer the English spelling), and generally enjoying it. My anaesthesia attending says that it is more important to know your anesthesiologist's credentials and understand what's involved in that aspect of a case as opposed to the surgeon, but after watching a CT surgeon do (surgere? surgerize?) a 6-hr, off-pump CABG on a 81-years-young patient, I'm not so sure. Both are important, I expect.
Seeing Sid Schwab and Scalpel as well as "old pal" platypus comment on my blog is nice. Thanks!
We had another VIP today at Metropolitan Medical Center, coming in for a 2 month old subacute subdural hematoma--a little out of the range (3 weeks) for subacute vs chronic, but that walked and talked like a subacute. Story goes, she (director of nursing for psychiatry, a nice lady and I trust her) was involved in a bad car wreck 2 months back, with her husband unfortunately receiving some pretty nasty lower extremity fractures. She got a nasty bump on her head along with some nausea/vomiting, and after the CT was read as normal, she was diagnosed with postconcussion syndrome. In the intervening two months, while her husband was being worked up for his fractures, she supported him while quietly cataloging and circular-filing her own symptoms, which included transient recurrent minor weakness in her left leg, transient numbness/tingling in her left arm, and an intruiging strip of paresthesia starting from the lateral canthus of her right eye and extending laterally into her scalp, not associated with tearing or dry eye. No N/V since then, no syncope, no cardiopulmonary symptoms, no seizures, no decreased level of consciousness.
[intermission: while these findings constitute focal neurologic signs, thus excluding PCS, I can imagine how, even in an experienced nurse, such a "diagnosis" can lead someone to minimize their symptoms until they become an impairment--"Oh, it's just my PCS acting up".]
[intermission #2: Nurses give great histories! This was like taking report on a patient instead of grinding out a history. VIP's are nice, for this and more reasons--they speak English, know their meds, know their history, and aren't afraid of mentioning things that other people would think the doctor "didn't need to know," like that bad reaction they had to penicillin 30 years ago resulting in an ICU stay, because medicine has really progressed since then, right?]
[there is NO intermission #3]
Being that the patient's regular doc was on vacation, she worked her grapevine to get expedited through the ER via my-favorite-attending, stopping by the CT and MRI machines for what she believed to be a transient ischemic attack, or mini-stroke. Well, she ended up fast-tracked to neurosurgery, where I saw her.
After a good deal of hand-patting, visits from our innumerable VP's and anxious relatives (uh, I mean, cowworker nurses), and a closed-session pep-talk by my anaestheia attending (who says anaesthesiologists don't talk to patients?), we got underway. After we had intubated and got some lines started, we waited around for the neurosurgeon awhile (sigh.). Finally the neurosurgery physician assistant comes in and immediately starts yelling! at my senior attending, for current and previous imagined slights! Agog, I stare unbelieving at this joker while he rants and whines about my attending for imagined slights (she wanted to talk to the surgeon about the case instead of this flunky) and finally leaves in a drama-queen huff. I mean, what is up with neurosurg PA's? They all seem to have a chip on their shoulder the size of Manhattan.
After the (rather young, given the 8-year residency neurosurgeon had come in and received his dose of abuse from the PA (while I again am shocked, chagrined, and stupefied at his impertinence. In the OR!), the surgery began. Nicely routine, with an interesting sidenote of how a subacute subdural will form a membrane around itself, leading to reformation of the hematoma despite every effort to prevent it. The surgeon explained that there is no way to prevent this, because stripping this extra membrane actually leads to increased recurrence of subdurals, and there is no way to "make the brain expand", like you would for a chronic pulmonary effusion to prevent recurrence. Long story short, the neurosurgeon started with Burr holes to evacuate the hematoma, and finding mainly solid hematoma, had to take out a chunk of skull to evacuate it, but otherwise the procedure went well, about 3 hours from the first cut.
After a teeth-grinding wait for transportation, I went and found a monitor myself after repeated overhead calls for a monitor (apparently VIP status doesn't faze the nursing attendants, of whom I've heard tell that if they stand up too fast they pass out. Trust an ER doc to do it himself. After that, our VIP went to recovery in the surgical intensive care unit, safe in the capable and caring hands of our SICU nurses.
Thursday, August 24, 2006
Being Insensitive and Evasive!
My presentation I made in a few hours on "breaking bad news," following the 10/20/30 rule of Powerpoint Presentations. The audience was interns and residents at my "continuity care", part of my internship:
Breaking Bad News
Dr. Dex--Metropolitan Medical Center
Problem
Paternalistic approach
Patient's Right of Autonomy and Self-Determination
Evaluating My Own Response
Bad Outcomes—Neglect & Misunderstanding
Physician Unprepared
Balancing Informing and Empathy
Pt feelings—Abandonment, Isolation, Confusion
Lack of Follow-up
Solution
What Do We Want?
Informed Patient
Independently Seeks Solutions
Communicates Problems, Complaints
Good Follow-Up
Support Network
Maximize Quality of Life
Maximize Normal Functioning
Advance Care Directives
ABCDE!
Advance Preparation
Arrange for Adequate Time, Privacy, and No Interruptions
Review Relevant Clinical Information
Mentally Rehearse, Phrases to Use/Avoid
Prepare Yourself Emotionally
Build a Therapeutic Relationship
What does the patient know/want to know?
Have family/support persons present
Introduce yourself to everyone
Warn the patient that bad news is coming
Use touch when appropriate
Schedule Follow-Up.
Communicate Well
Ask what the patient knows
Be “Frank” but Compassionate—avoid jargon and euphemisms
Allow for Silence and Tears; Patient's pace
Ask Patient to Verbalize Understanding
Allow Time to Answer Questions
Conclude with Summary and Plan
Deal With Patient and Family Reactions
Assess and Respond to Patient and Family Emotional Reactions; repeat at each Visit
Be Empathetic
Do not Argue With or Criticize Colleagues (including in notes!)
Encourage and Validate Emotions
Explore What the News Means to the Patient
Offer Realistic Hope according to the Patient's Goals
Use Interdisciplinary Resources
Take Care of Your Own Needs; Be attuned to the Needs of involved House Staff and Office or Hospital Personnel.
Mistakes to Avoid
Patient Confused As To Diagnosis or Plan.
Patient in Denial or Not on Board
Neglected Getting Professional Translation
Other caregivers unaware of diagnosis (ER!)
Pt in Pain or with Unresolved Questions
No Advance Care Directive
Patients' diagnosis minimized
Patient's reaction to diagnosis explored
My Own Tips
Sit Down
Make sure you're right
Confirm and Name (“Mirror”) Patient's Emotions
Delegate One Family Member
Get Translation
The Patient Is the One with The Disease
Ensure Pain Control
Ensure Medical Follow-Up
Ensure Ancillary Services—SW, Financial, Hospice, ER Packet, Support Group,
ABCDE!
Advance preparation
Build a therapeutic environment/relationship
Communicate Well
Deal with Patient and Family Reactions
Encourage and Validate Emotions
What do you think?
-The Emergencist
Breaking Bad News
Dr. Dex--Metropolitan Medical Center
Problem
Paternalistic approach
Patient's Right of Autonomy and Self-Determination
Evaluating My Own Response
Bad Outcomes—Neglect & Misunderstanding
Physician Unprepared
Balancing Informing and Empathy
Pt feelings—Abandonment, Isolation, Confusion
Lack of Follow-up
Solution
What Do We Want?
Informed Patient
Independently Seeks Solutions
Communicates Problems, Complaints
Good Follow-Up
Support Network
Maximize Quality of Life
Maximize Normal Functioning
Advance Care Directives
ABCDE!
Advance Preparation
Arrange for Adequate Time, Privacy, and No Interruptions
Review Relevant Clinical Information
Mentally Rehearse, Phrases to Use/Avoid
Prepare Yourself Emotionally
Build a Therapeutic Relationship
What does the patient know/want to know?
Have family/support persons present
Introduce yourself to everyone
Warn the patient that bad news is coming
Use touch when appropriate
Schedule Follow-Up.
Communicate Well
Ask what the patient knows
Be “Frank” but Compassionate—avoid jargon and euphemisms
Allow for Silence and Tears; Patient's pace
Ask Patient to Verbalize Understanding
Allow Time to Answer Questions
Conclude with Summary and Plan
Deal With Patient and Family Reactions
Assess and Respond to Patient and Family Emotional Reactions; repeat at each Visit
Be Empathetic
Do not Argue With or Criticize Colleagues (including in notes!)
Encourage and Validate Emotions
Explore What the News Means to the Patient
Offer Realistic Hope according to the Patient's Goals
Use Interdisciplinary Resources
Take Care of Your Own Needs; Be attuned to the Needs of involved House Staff and Office or Hospital Personnel.
Mistakes to Avoid
Patient Confused As To Diagnosis or Plan.
Patient in Denial or Not on Board
Neglected Getting Professional Translation
Other caregivers unaware of diagnosis (ER!)
Pt in Pain or with Unresolved Questions
No Advance Care Directive
Patients' diagnosis minimized
Patient's reaction to diagnosis explored
My Own Tips
Sit Down
Make sure you're right
Confirm and Name (“Mirror”) Patient's Emotions
Delegate One Family Member
Get Translation
The Patient Is the One with The Disease
Ensure Pain Control
Ensure Medical Follow-Up
Ensure Ancillary Services—SW, Financial, Hospice, ER Packet, Support Group,
ABCDE!
Advance preparation
Build a therapeutic environment/relationship
Communicate Well
Deal with Patient and Family Reactions
Encourage and Validate Emotions
What do you think?
-The Emergencist
Monday, August 21, 2006
Your Safe Place draft
One of the good things about learning so much psychology and psychiatry like I did is when you switch to ER like I'm doing is that I can be a stealth psychiatrist or psychologist. How? Let me count the ways I used psych today:
When I deal with a psych patient, I know what to ask about besides, "uh, do you want to kill yourself? How about other people? Yes, okay. A "special" doctor will see you now. GOODBYE! Don't ever talk to me again. No I'm not giving you any pain medicine, see, cuz you're a PSYCH patient. That means I don't have to talk to you. That means you wait the longest.
I know that psych pts (they wear pink-orange gowns in my ER) get physical diseases. I know how to talk to them. Literal use of metaphor, and sprinkle in the important bits in your creamy conversation monologue like the rice crunches in a Toblerone.
I seem to get more VIPs, lubricated by a PCT or a Pt rep or a pushy relative. No problem, ma'am, I'll see to it immediately. I'm like a soothing salve on the festering wound of modern medical care. I don't care, I'm an intern. And I'm rotating. I'll take the time to extract your history, even the touchy parts like genital complaints or worsening mental status or desperate social situations, like a car service voucher from the ER at 3:00 AM, and I'll make sure they're dealt with.
I get a better history. Hands down.
I alsways get a translator, because most medical errors come from communication breakdown.
I believe you are in pain. I'll treat you for it even though I think you're hysterically maximizing your pain (hispanics, I'm looking at you), because pain is subjective.
There are other methods of pain control besides "ten pounds of mofeen". Today, I talked down a screaming gallbladder with pancreatitis into counting her breaths enough to get an EKG. After I scraped her down from the ceiling.
Pelvic/rectal exams--professional and gentle.
I tell you what I'm thinking if I think you can take it, cuz it motivates you to stay and get proper treatment.
I'll try and rescue you from "00-doctors"--PMD's with HMO contracts.
No problem too small for a complete H & P. I expect "doorknob" phenomenon in these patients--"By the way, about this chest pain I've been having..."
I've got a clinic, cuz my profession (D.O.'s, osteopaths) believe in primary care. I will see you there. I'm conscientious and thorough.
Nurses of my patients know I appreciate their efforts. I encourage patients to get to know their nurses.
Going to the ER is a big deal. I know you wouldn't come unless you think it's serious. Unless it isn't, but I make that decision.
Dx and tx are equal or secondary to patient's understanding of their condition and the gravity they comprehend from my assessment and explanation. If they don't know, they can't tell the next Dr. to see them, right?
smiling is healty. I make you smile during every physical. (to test for facial droop. Fun test, eh?)
I still haven't mastered legitimately irate or frustrated patients, becuase I understand their situation and sympathize with their gnashing outrage at unnecessary delays.
I would choose me for my dr.
do good and be happy!
Signing off,
--the emerencist.
When I deal with a psych patient, I know what to ask about besides, "uh, do you want to kill yourself? How about other people? Yes, okay. A "special" doctor will see you now. GOODBYE! Don't ever talk to me again. No I'm not giving you any pain medicine, see, cuz you're a PSYCH patient. That means I don't have to talk to you. That means you wait the longest.
I know that psych pts (they wear pink-orange gowns in my ER) get physical diseases. I know how to talk to them. Literal use of metaphor, and sprinkle in the important bits in your creamy conversation monologue like the rice crunches in a Toblerone.
I seem to get more VIPs, lubricated by a PCT or a Pt rep or a pushy relative. No problem, ma'am, I'll see to it immediately. I'm like a soothing salve on the festering wound of modern medical care. I don't care, I'm an intern. And I'm rotating. I'll take the time to extract your history, even the touchy parts like genital complaints or worsening mental status or desperate social situations, like a car service voucher from the ER at 3:00 AM, and I'll make sure they're dealt with.
I get a better history. Hands down.
I alsways get a translator, because most medical errors come from communication breakdown.
I believe you are in pain. I'll treat you for it even though I think you're hysterically maximizing your pain (hispanics, I'm looking at you), because pain is subjective.
There are other methods of pain control besides "ten pounds of mofeen". Today, I talked down a screaming gallbladder with pancreatitis into counting her breaths enough to get an EKG. After I scraped her down from the ceiling.
Pelvic/rectal exams--professional and gentle.
I tell you what I'm thinking if I think you can take it, cuz it motivates you to stay and get proper treatment.
I'll try and rescue you from "00-doctors"--PMD's with HMO contracts.
No problem too small for a complete H & P. I expect "doorknob" phenomenon in these patients--"By the way, about this chest pain I've been having..."
I've got a clinic, cuz my profession (D.O.'s, osteopaths) believe in primary care. I will see you there. I'm conscientious and thorough.
Nurses of my patients know I appreciate their efforts. I encourage patients to get to know their nurses.
Going to the ER is a big deal. I know you wouldn't come unless you think it's serious. Unless it isn't, but I make that decision.
Dx and tx are equal or secondary to patient's understanding of their condition and the gravity they comprehend from my assessment and explanation. If they don't know, they can't tell the next Dr. to see them, right?
smiling is healty. I make you smile during every physical. (to test for facial droop. Fun test, eh?)
I still haven't mastered legitimately irate or frustrated patients, becuase I understand their situation and sympathize with their gnashing outrage at unnecessary delays.
I would choose me for my dr.
do good and be happy!
Signing off,
--the emerencist.
Friday, August 18, 2006
VIPs are not immune to medical dehumanization
I had mistakenly picked up a VIP, after my attending told me to pick up "Lauren Barkerson" (Sigh. After all the trouble I take to camouflage my identity, location, and hopsital, still you doubt.) I instead picked up Leroy Schneerson, and spent a goodly time poring over his previous visits and the triage note. Triage notes a 72 year old with a 1.5 week history of GI bleeding. PMHx: s/p colonoscopy today AM (it was about 7:45 P.M.), 'tics, CAD, high chol, DM2, yadda yadda yadda. After ordering triage labs that were conspicuously absent, 'specially type and screen, EKG, CXR, "ER Belly labs," (CBC, Chem 7, Amyl, Lip, Pt/Ptt, Liver profile, and, mysteriously enough, Lipid profile (yeah, like we're gonna start statins on a single, sick, unknown fasting state lipid profile.)) and "ER CP labs (Most of the above plus trops, "CKAxsymb" and myoglobin.) (yeah, no ESR or CRP. whatever.) Then I look up to eyeball the patient. Uh. Looks like I'm walking on eggshells for awhile. The salty patient representative (very helpful to have) comes up and says, "You gotta go see this guy. He's a bigshot local judge, a VIP". As I go over to see him, I get an overhead page for a phone call. Huh? I din't page any one. Did I? NVM. "Dr. Emergencist here." "This is Dr. Important. I did the colonoscopy this morning." "Oh, okay. Well, he's slightly hypotensive, and I've got a note from the PMD Dr. Influence saying he's dropped his crit from 35 to 23 in a week. He's a little hypotensive (104/56) but he looks AAOx3." "Okay, document his guiac and get a [6 hour GI bleed nuclear scan]". "...okay...what's that?" (I'm deciding he know's I'm a tern, and play it to the hilt.) "It localizes GI bleeding as little as 0.1 ml." I'm thinking, wow, sounds cool, but, gee, don't think my attending will go for it. "sure thing, Dr. Important. Soon as I evaluate him." The patient had been in the ER for 1.5 hours after triage by now. So I go to see him, when my attending says, "hey you din't pick up that patient I asked you to." "umm, yes I did. Leroy Schneerson. VIP--GI Dr. Important called ME!" "No, go see the original patient I wanted you to see first. She's been waiting 2 hours" Hmm. I look at VIP, primed to evaluate him and finesse the situation--no such luck. About face back to the tracking board. This one is 79 and "generalized weakness". Crap. Oh, and a h/o neurofibromatosis and afib. ? Uh, okay, I'm sure there's something perfectly obvious and slam-dunk for me, so I can get to VIP. I don't want administrators, irate private attendings, and belligerent relatives breathing down my neck as I go see a different patient. So I'm juggling diagnosis and management of two complicated elderly patients, something a
Wicked!
X-posted from a comment on this post by Nurse Kim/Emergiblog:
Heh. Wait'll you get a load of me. Here goes:
Now I must engage a profound issue or struggle or confusion or consternation of modernity.
I confess, like many such young, inexperienced, greenhorn, of-the-all-thumbs doctors, I am male.
Here's a picture of me in my shaggy days
As such, unless I engage in such banter, first-name-basisness, familiarity, shameless praise, jocularity, obsequiousness, black medical humor, unbelievably contorted expressions of sympathy, affected apparent world-weariness and the distant far-seeing horizon-scanning characteristic of rugged, craggy, uncompromising ownership of turf in my ward, (ER excepted: All those participating in the care of the mind-numbingly abusive, recalcitrant, and unwieldly subset of humanity that presents to my ER on a torrential basis automatically are allied and united against them) the nurses will thereupon commence to "train," "educate," "be-spine-ify," and otherwise mercilessly and cruelly torture "The Intern" thusly:
1. The infamous "Tylenol call": [15 minutes after innocently, sympathetically bundling the deliriously bleary-eyed intern off to bed, amazingly exactly the moment after head hits pillow, during satisfied exhalation of blissful relaxation--after a 2-hour fruitless code and 1-hour marathon harangue by enraged relatives at the worthless so-called-doctor who killed their beloved Grandma] "Um, so sorry to BOTHER you, DOCTOR, but poor Mrs. Potts in Bed 15 A had a headache, and you know how thin her blood is, and I was wondering if I could just give her a tylenol to take the edge off?" [fully knowing that the nearly-demented intern, having taken an incoherent 10-second sign-out on the patient 8 long hours ago, vaguely remembers something about a questionable intracranial hemmorhage on CT 8 years previously in this completely demented 89 year old female, and thus is obligated to extricate himself from ecstacy of pillow and bed, dragging himself to evaluate at the bedside this abusive, violently bitter old hag for headache.]
2. Strategic use of refusal to bedpan/blood culture/maintain a ventilator/start a medicated drip based on obscure citatations of "hospital/union policy" .
3. Careful application of selective incompetence, especially with respect to IV's, nasogastric tubes, dressing changes, and multiple demanding family members.
4. Sequential scheduled breaks at the start of visiting hours, resulting in multiple nursing hand-offs and complete hysterical breakdown of hapless intern while running about trying to find nurses, techs, hell, ANYBODY, to change diapers and prepare bedpans for every patient on the floor finally, or in some cases, mysteriously, receiving simultaneous bowel clean out [Golytely = projectile diarrhea] and long-ignored, subsequently more and more powerful laxative orders. Utter perfection.
5. Reporting critical laboratory findings, pathology reports, and changes in clinical status only to attendings, and carrying out subsequent orders without notifying interns, consequently rendering the by now twitching and wretched intern completely out of the loop of actual medical care, appearing hopelessly incompetent to superiors. Ah, sweet victory.
6. Complete, total, and jealous ownership of every tech/housekeeper/computer geek/social worker, all medical supplies, and every actually working critical piece of office equipment behind assinine coded doors.
...
My question is, how does this process change if the doctor is female, single, and good-looking?
--the Emergencist
Disrupting Delicate Constitutions 24/7.
Rumor has it that “The Answer Nurse” will be touring, once again to be interviewed here at Emergiblog!
So think of all the questions you always wanted to ask a nurse but were afraid to know. The Answer Nurse requests that only questions denoting a proper social demeanor be posed, as anything of an inappropriate nature disrupts her delicate constitution.
Heh. Wait'll you get a load of me. Here goes:
Now I must engage a profound issue or struggle or confusion or consternation of modernity.
I confess, like many such young, inexperienced, greenhorn, of-the-all-thumbs doctors, I am male.
Here's a picture of me in my shaggy days
As such, unless I engage in such banter, first-name-basisness, familiarity, shameless praise, jocularity, obsequiousness, black medical humor, unbelievably contorted expressions of sympathy, affected apparent world-weariness and the distant far-seeing horizon-scanning characteristic of rugged, craggy, uncompromising ownership of turf in my ward, (ER excepted: All those participating in the care of the mind-numbingly abusive, recalcitrant, and unwieldly subset of humanity that presents to my ER on a torrential basis automatically are allied and united against them) the nurses will thereupon commence to "train," "educate," "be-spine-ify," and otherwise mercilessly and cruelly torture "The Intern" thusly:
1. The infamous "Tylenol call": [15 minutes after innocently, sympathetically bundling the deliriously bleary-eyed intern off to bed, amazingly exactly the moment after head hits pillow, during satisfied exhalation of blissful relaxation--after a 2-hour fruitless code and 1-hour marathon harangue by enraged relatives at the worthless so-called-doctor who killed their beloved Grandma] "Um, so sorry to BOTHER you, DOCTOR, but poor Mrs. Potts in Bed 15 A had a headache, and you know how thin her blood is, and I was wondering if I could just give her a tylenol to take the edge off?" [fully knowing that the nearly-demented intern, having taken an incoherent 10-second sign-out on the patient 8 long hours ago, vaguely remembers something about a questionable intracranial hemmorhage on CT 8 years previously in this completely demented 89 year old female, and thus is obligated to extricate himself from ecstacy of pillow and bed, dragging himself to evaluate at the bedside this abusive, violently bitter old hag for headache.]
2. Strategic use of refusal to bedpan/blood culture/maintain a ventilator/start a medicated drip based on obscure citatations of "hospital/union policy" .
3. Careful application of selective incompetence, especially with respect to IV's, nasogastric tubes, dressing changes, and multiple demanding family members.
4. Sequential scheduled breaks at the start of visiting hours, resulting in multiple nursing hand-offs and complete hysterical breakdown of hapless intern while running about trying to find nurses, techs, hell, ANYBODY, to change diapers and prepare bedpans for every patient on the floor finally, or in some cases, mysteriously, receiving simultaneous bowel clean out [Golytely = projectile diarrhea] and long-ignored, subsequently more and more powerful laxative orders. Utter perfection.
5. Reporting critical laboratory findings, pathology reports, and changes in clinical status only to attendings, and carrying out subsequent orders without notifying interns, consequently rendering the by now twitching and wretched intern completely out of the loop of actual medical care, appearing hopelessly incompetent to superiors. Ah, sweet victory.
6. Complete, total, and jealous ownership of every tech/housekeeper/computer geek/social worker, all medical supplies, and every actually working critical piece of office equipment behind assinine coded doors.
...
My question is, how does this process change if the doctor is female, single, and good-looking?
--the Emergencist
Disrupting Delicate Constitutions 24/7.
Tres Hombres En Italia

From Top right, clockwise: The "REAL" Cheerful Oncologist, The Uncarved Block, and A Budding Emergencist. Viva Venezia!

From Top right, clockwise: The "REAL" Cheerful Oncologist, The Uncarved Block, and A Budding Emergencist. Viva Venezia!
Sunday, August 13, 2006
Are Toxidromes interesting? Yup.
I have always seen
Like the AEIOU mnemonic for indications for emergent dialysis.
Another pearl I picked up today--end-stage renal patients, in addition to accumulating electrolyte disturbances like they were on the clearance rack, also have no way to eliminate fluids. Duh. So they show up on your doorstep in pulmonary edema from volume overload. BNP>1000 not uncommon for walkie-talkies, of course in addition to K+ over 7 and creatinines hovering around 10 as their blood becomes more urine than plasma.
Today we got notified of a 27 year old, coming in with an OD of, wait for it, wait for it...chloral hydrate.
Huh?
Yeah. It was bad, too. Breathing at 6 per minute. Comatose, unresponsive to prehospital D50 and Narcan. 1/4 full 400ml bottle of chloral hydrate (AKA "Mickey Finns" when combined with alcohol, until recently used for conscious sedation in the ER, in the 50's for insomnia, and as a surgical anaesthic in the distant past. Why the hell does she have it?) on the stretcher. Pupils miotic and nonreactive. Hypotensive. BGM wnl. GCS 4. Intubate! 40 of etomidate and 200 of sux. Go!
Husband, the precipitant for said OD, comes into resuscitation bay amid the chaos. He has obviously been crying, but is looking for a fight, arms akimbo, looking for someone to blame, watching as 4 doctors, 3 nurses, an RT and 2 medical students (quiet, out of the way, and wanting to help, like good little med students) manage the resuscitation. Oh, hell, no. Get out! He, shocked and hurt, returns to ambulatory triage where his guilt and shame ambush him. The second year struggles not to intubate the esophagus, calling out, "I see vallecula, I don't, I do, I don't," etc.). Finally, tube is in, resps in lungs. Good. Meanwhile the nurse has been Foleyifying her; at this point this waif is completely exposed. I'm watching and discussing the toxidrome with CHILL-AS-FRICK ATTENDING, while GOOD-TEACHER-ATTENDING leads the code. Meanwhile, HOPELESS PRICK ATTENDING (my supervisor for the day, grr) sees my 18 yr old upper middle class, 5 months pregnant, strangely without prenatal care, with abdo pain (eventually a UTI, which I knew at the time). I turn to present, stop for a sec, and turn back to the much more interesting resuscitation. Our pride in our 2nd year resident for successfully intubating the pt melts as results to our shotgun initial orders come back. Blood gas--metabolic acidosis with adequate and expected respiratory compensation (pH 7.3, which I would judge as expected given the patient's crashing, and actually encouraging). Normal anion gap. Chem essentialy normal except for the aforementioned low bicarb. A pregnant pause. "What do we know about chloral hydrate tox?" says GOOD-TEACHER-ATTENDING, in more of a "I don't know" tone than "Do you know?" one. Um. I whip out my trusty palm. "hypotension. Seizures. Leukopenia. N/V, diarrhea, and sleep walking," I lamely mumble. I seize upon seizures, and fire off questions about sz at the paramedic. Nope. I return to my gigantic, expensive, and supposedly comprehensive palm programs futilely.
The precise mechanism of action of chloral hydrate is unknown but is confined to the cerebral hemispheres (Sifton, 1998). It is a general central nervous system depressant with minimal analgesic effects and a low ratio of anticonvulsant to sedative effects. Chloral hydrate decreases sleep latency and nighttime awakenings with minimal effects on REM sleep (Gilman et al, 1985).
The toxidrome involves respitory depression, life-threatenting arrhythmias, possible seizures, and coma or obtundation (half-life of 4-9 hours). Does it have tricyclic-like activity? According to my lit review (keyword: "chloral hydrate overdose" on medline), it acts like a benzo. In our case, given the development of wide-complex tachycardia, and reversal following 2 amps of sodium bicarb (an amp of socium bicarb is 3% sodium as compared with 0.9% in normal saline
Flumazenil is a competitive antagonist with specific action at the central benzodiazepine receptor. It is used when benzodiazepine intoxication is suspected. Its use has also been reported in cannabis intoxication, chloral hydrate overdose, hepatic encephalopathy, and alcohol intoxication.
Like the AEIOU mnemonic for indications for emergent dialysis.
Another pearl I picked up today--end-stage renal patients, in addition to accumulating electrolyte disturbances like they were on the clearance rack, also have no way to eliminate fluids. Duh. So they show up on your doorstep in pulmonary edema from volume overload. BNP>1000 not uncommon for walkie-talkies, of course in addition to K+ over 7 and creatinines hovering around 10 as their blood becomes more urine than plasma.
Today we got notified of a 27 year old, coming in with an OD of, wait for it, wait for it...chloral hydrate.
Huh?
Yeah. It was bad, too. Breathing at 6 per minute. Comatose, unresponsive to prehospital D50 and Narcan. 1/4 full 400ml bottle of chloral hydrate (AKA "Mickey Finns" when combined with alcohol, until recently used for conscious sedation in the ER, in the 50's for insomnia, and as a surgical anaesthic in the distant past. Why the hell does she have it?) on the stretcher. Pupils miotic and nonreactive. Hypotensive. BGM wnl. GCS 4. Intubate! 40 of etomidate and 200 of sux. Go!
Husband, the precipitant for said OD, comes into resuscitation bay amid the chaos. He has obviously been crying, but is looking for a fight, arms akimbo, looking for someone to blame, watching as 4 doctors, 3 nurses, an RT and 2 medical students (quiet, out of the way, and wanting to help, like good little med students) manage the resuscitation. Oh, hell, no. Get out! He, shocked and hurt, returns to ambulatory triage where his guilt and shame ambush him. The second year struggles not to intubate the esophagus, calling out, "I see vallecula, I don't, I do, I don't," etc.). Finally, tube is in, resps in lungs. Good. Meanwhile the nurse has been Foleyifying her; at this point this waif is completely exposed. I'm watching and discussing the toxidrome with CHILL-AS-FRICK ATTENDING, while GOOD-TEACHER-ATTENDING leads the code. Meanwhile, HOPELESS PRICK ATTENDING (my supervisor for the day, grr) sees my 18 yr old upper middle class, 5 months pregnant, strangely without prenatal care, with abdo pain (eventually a UTI, which I knew at the time). I turn to present, stop for a sec, and turn back to the much more interesting resuscitation. Our pride in our 2nd year resident for successfully intubating the pt melts as results to our shotgun initial orders come back. Blood gas--metabolic acidosis with adequate and expected respiratory compensation (pH 7.3, which I would judge as expected given the patient's crashing, and actually encouraging). Normal anion gap. Chem essentialy normal except for the aforementioned low bicarb. A pregnant pause. "What do we know about chloral hydrate tox?" says GOOD-TEACHER-ATTENDING, in more of a "I don't know" tone than "Do you know?" one. Um. I whip out my trusty palm. "hypotension. Seizures. Leukopenia. N/V, diarrhea, and sleep walking," I lamely mumble. I seize upon seizures, and fire off questions about sz at the paramedic. Nope. I return to my gigantic, expensive, and supposedly comprehensive palm programs futilely.
The precise mechanism of action of chloral hydrate is unknown but is confined to the cerebral hemispheres (Sifton, 1998). It is a general central nervous system depressant with minimal analgesic effects and a low ratio of anticonvulsant to sedative effects. Chloral hydrate decreases sleep latency and nighttime awakenings with minimal effects on REM sleep (Gilman et al, 1985).
The toxidrome involves respitory depression, life-threatenting arrhythmias, possible seizures, and coma or obtundation (half-life of 4-9 hours). Does it have tricyclic-like activity? According to my lit review (keyword: "chloral hydrate overdose" on medline), it acts like a benzo. In our case, given the development of wide-complex tachycardia, and reversal following 2 amps of sodium bicarb (an amp of socium bicarb is 3% sodium as compared with 0.9% in normal saline
Flumazenil is a competitive antagonist with specific action at the central benzodiazepine receptor. It is used when benzodiazepine intoxication is suspected. Its use has also been reported in cannabis intoxication, chloral hydrate overdose, hepatic encephalopathy, and alcohol intoxication.
Friday, August 11, 2006
The Road to Hell...

Cross posted from a comment about this shining example of misguided intentions, from Dr. Parker at A Chance to Cut...
Do ppl think of that guy in Grey's Anatomy when they think of neurosurgeon? D'ya remember he drove a Jeep and lived in a trailer? An it's not just the doctor. More often than not in cases of necessity and dire financial straits, a doctor will negotiate or waive fees altogether, like my father, who is one of the only oncologists in his area, and treats everybody. Of course, without renumeration, nurses, techs, janitors, billers, and security guards will not show up to work. Electricity will not cauterize bleeding vessels, equipment will not be sterile, and x-rays will not magically appear out of thin air. It is an enormous commitment of manpower and materiel to maintain a L1 trauma center. I overheard that simply activating the trauma team costs $5,000, whether it is a drunk-fall-down-go-boom or a young mother-hit-by-a-stray-bullet.
I think tha problem has to do with the fact that nobody has any idea of what things cost in medicine. I get bits and pieces here and there, like suture costs around $10 a pack, an implantable pacemaker/cardiodefibrillator costs $30,000 (just the device!), and a venous access graft for dialysis costs upwards of $5,000.
Doctors, as a rule, rarely discuss costs with a patient. We may pat ourselves on the back for giving a $12 antibiotic versus a $50 one, but it's really peanuts compared to labor and maintenance in an intensely labor-intensive environment such as an ICU, or a course of chemo. The reason why we don't discuss payment, why we as physicians avoid even finding out how much things cost until WE'RE paying for it, is that many patients would refuse treatment. Most medical treatments are painful and scary enough without them costing a fortune--the only difference between a poison and a drug is the dose.
Now, in China, people gotta pay up front. I think that's the way of things here with specialty stuff, like child psychiatry or a scheduled c-section, or other planned procedures. China beats us at our own game of merciless mercantilism, and coupled with a populatio of 1 Billion kind of makes life, and suffering, cheap. Here we crucify our greedy, arrogant doctors who let gomertose, vent-dependent patients die during a F#!%@#$ HURRICANE--as the water creeps up over your knees, nowhere to go, no help in sight, people with guns...believe me, you. would. do. the. same. precious principles be damned But it's still "DAMN THE TORPEDOES!" when it comes to costs in the ER.

Cross posted from a comment about this shining example of misguided intentions, from Dr. Parker at A Chance to Cut...
Do ppl think of that guy in Grey's Anatomy when they think of neurosurgeon? D'ya remember he drove a Jeep and lived in a trailer? An it's not just the doctor. More often than not in cases of necessity and dire financial straits, a doctor will negotiate or waive fees altogether, like my father, who is one of the only oncologists in his area, and treats everybody. Of course, without renumeration, nurses, techs, janitors, billers, and security guards will not show up to work. Electricity will not cauterize bleeding vessels, equipment will not be sterile, and x-rays will not magically appear out of thin air. It is an enormous commitment of manpower and materiel to maintain a L1 trauma center. I overheard that simply activating the trauma team costs $5,000, whether it is a drunk-fall-down-go-boom or a young mother-hit-by-a-stray-bullet.
I think tha problem has to do with the fact that nobody has any idea of what things cost in medicine. I get bits and pieces here and there, like suture costs around $10 a pack, an implantable pacemaker/cardiodefibrillator costs $30,000 (just the device!), and a venous access graft for dialysis costs upwards of $5,000.
Doctors, as a rule, rarely discuss costs with a patient. We may pat ourselves on the back for giving a $12 antibiotic versus a $50 one, but it's really peanuts compared to labor and maintenance in an intensely labor-intensive environment such as an ICU, or a course of chemo. The reason why we don't discuss payment, why we as physicians avoid even finding out how much things cost until WE'RE paying for it, is that many patients would refuse treatment. Most medical treatments are painful and scary enough without them costing a fortune--the only difference between a poison and a drug is the dose.
Now, in China, people gotta pay up front. I think that's the way of things here with specialty stuff, like child psychiatry or a scheduled c-section, or other planned procedures. China beats us at our own game of merciless mercantilism, and coupled with a populatio of 1 Billion kind of makes life, and suffering, cheap. Here we crucify our greedy, arrogant doctors who let gomertose, vent-dependent patients die during a F#!%@#$ HURRICANE--as the water creeps up over your knees, nowhere to go, no help in sight, people with guns...believe me, you. would. do. the. same. precious principles be damned But it's still "DAMN THE TORPEDOES!" when it comes to costs in the ER.
Sam Stone in the ER
Inspired by this post, which is actually light hearted by The Platypus:
Sam Stone came home,
To his wife and family
After serving in the conflict overseas.
And the time that he served,
Had shattered all his nerves,
And left a little shrapnel in his knee.
But the morphine eased the pain,
And the grass grew round his brain,
And gave him all the confidence he lacked,
With a Purple Heart and a monkey on his back.
There's a hole in daddy's arm where all the money goes,
Jesus Christ died for nothin' I suppose.
Little pitchers have big ears,
Don't stop to count the years,
Sweet songs never last too long on broken radios.
Mmm....
Sam Stone's welcome home
Didn't last too long.
He went to work when he'd spent his last dime
And Sammy took to stealing
When he got that empty feeling
For a hundred dollar habit without overtime.
And the gold rolled through his veins
Like a thousand railroad trains,
And eased his mind in the hours that he chose,
While the kids ran around wearin' other peoples' clothes...
Sam Stone was alone
When he popped his last balloon
Climbing walls while sitting in a chair
Well, he played his last request
While the room smelled just like death
With an overdose hovering in the air
But life had lost its fun
And there was nothing to be done
But trade his house that he bought on the G, I. Bill
For a flag draped casket on a local heroes' hill
--"Sam Stone" by John Prine, covered excellently by SWAMP DOGG
Sam Stone came home,
To his wife and family
After serving in the conflict overseas.
And the time that he served,
Had shattered all his nerves,
And left a little shrapnel in his knee.
But the morphine eased the pain,
And the grass grew round his brain,
And gave him all the confidence he lacked,
With a Purple Heart and a monkey on his back.
There's a hole in daddy's arm where all the money goes,
Jesus Christ died for nothin' I suppose.
Little pitchers have big ears,
Don't stop to count the years,
Sweet songs never last too long on broken radios.
Mmm....
Sam Stone's welcome home
Didn't last too long.
He went to work when he'd spent his last dime
And Sammy took to stealing
When he got that empty feeling
For a hundred dollar habit without overtime.
And the gold rolled through his veins
Like a thousand railroad trains,
And eased his mind in the hours that he chose,
While the kids ran around wearin' other peoples' clothes...
Sam Stone was alone
When he popped his last balloon
Climbing walls while sitting in a chair
Well, he played his last request
While the room smelled just like death
With an overdose hovering in the air
But life had lost its fun
And there was nothing to be done
But trade his house that he bought on the G, I. Bill
For a flag draped casket on a local heroes' hill
--"Sam Stone" by John Prine, covered excellently by SWAMP DOGG
Personal statement time!
Hello, world!
It's time for me to write my personal statement to apply for an EM residency next year!
Some things to remember when you are writing YOUR PS:
You want to give this impression:
And not this impression as a Personal Statement:

Or this one:

I've heard time and time again that your record, your history, is more examined than your personal statement. Your PS, and also your interview (YMMV) are to ascertain whether or not you have horns and a tail. Also to see if you have a pulse.
It's time for me to write my personal statement to apply for an EM residency next year!
Some things to remember when you are writing YOUR PS:
You want to give this impression:
And not this impression as a Personal Statement:

Or this one:

I've heard time and time again that your record, your history, is more examined than your personal statement. Your PS, and also your interview (YMMV) are to ascertain whether or not you have horns and a tail. Also to see if you have a pulse.
Tuesday, August 08, 2006
Digging In
Well, I've got six shifts coming up in the next seven days. The ER is great, I'm happy to be there, it's just that I get pretty tired after a 12-hr shift. Seems I have to sleep 12 hours just to make up for it.
Yesterday, CHIEF RESIDENT told me that about hours regulations in the ER. You may have heard about 405 regulations, where residents can't work more than 80 hours in a week, averaged over 2 weeks. Well, ER programs have taken it upon themselves to restrict residents' hours to 60 per week--the rationale being that working 60 hours in a week is like working 80 hours on the floors. Damn, so true.
I wish I had one of those portable phones that the upper level residents carry. I keep missing callbacks from consultants. Doesn't look good. Looks bad, in fact. One of the attendings I was considering asking for a letter of rec mentioned that I missed a call from a consultant. Well, scratch him off the list. I even told him why I missed it--I was getting a bite to eat. I had paged the consultant 1/2 an hour ago, and finally went to eat for 10 minutes. Crap.
On the up side, however, there is a fun, good looking patient representative I'm thinking about asking out. We'll see.
Yesterday, CHIEF RESIDENT told me that about hours regulations in the ER. You may have heard about 405 regulations, where residents can't work more than 80 hours in a week, averaged over 2 weeks. Well, ER programs have taken it upon themselves to restrict residents' hours to 60 per week--the rationale being that working 60 hours in a week is like working 80 hours on the floors. Damn, so true.
I wish I had one of those portable phones that the upper level residents carry. I keep missing callbacks from consultants. Doesn't look good. Looks bad, in fact. One of the attendings I was considering asking for a letter of rec mentioned that I missed a call from a consultant. Well, scratch him off the list. I even told him why I missed it--I was getting a bite to eat. I had paged the consultant 1/2 an hour ago, and finally went to eat for 10 minutes. Crap.
On the up side, however, there is a fun, good looking patient representative I'm thinking about asking out. We'll see.
Friday, August 04, 2006
Whoa. Keanu Reeves style.
An incredible 7-part series on a ruptured AAA from an Australian surgical resident(Abdominal Aortic Aneurysm), via Grand Rounds, this week hosted by Inside Surgery.
Thursday, August 03, 2006
Letting my Idol down
I did two 12 hour shifts with my idol, CHIEF RESIDENT last weekend, and last night his swing shift partially coincided with mine. Some of my illusions were dashed when I overheard him saying, you know on Saturday I had 22 patients and on Sunday I had 25. That's way too much for a resident. With kind of a numb regret, or horror, I realized that I, on the same shifts, covering the same patients, had seen 7 or 8 each night. I had no idea of the lopsidedness of this equation, even grumbling to myself when, flushed with New Doctor Discovering His Value, he would tell me that he had assigned me a new patient. Grr, I thought, I'm working hard, can't he see that? I'll pick up a new patient when I'm good and ready. Little do I know.
The last two shifts, I humped hard, spurred by CHIEF RESIDENT's admonition that interns should see 10-12 patients per 12-hour shift. I was already working as hard as I could, I thought. Much of my time was spend figuring out how things were done, like how you have to order oral contrast separately if you order a gut CT, or worse, how I am still mystified by the computer's admission procedure, wasting my precious minutes and those of residents asking for help. I console myself, thinking, well, you'll learn to run those computer gears until they hum. I console myself, because I know eventually pressure for THROUGHPUT will eat away at time I use consoling, explaining, and cajoling patients into, through, and and after their ED visits.
I think of the time that I didn't take explaining to a kindly 61 year old postman, who I had seen 2 shifts earlier in the ER, returning with the same problem, urinary retention (which I ultimately discovered was due to not BPH or some horrible abdominal pathology, but just a stupid stone), now with an uncomfortable leg bag an indwelling foley penis catheter, placed by my idol, CHIEF RESIDENT, in a misguided attempt to avoid uremia, while not getting the test that would have simplified everything, a CT abdo) and his darling, caring wife, about his uric acid kidney stones and how to avoid them, because that's for his primary medical doctor, isn't it? Only, this couple is new to the medical game and is UNCLEAR ON THE CONCEPT of private physicians for people with good insurance, and gov't insurance is superb. So he will go to whatever shmuck intern will see him in the clinic, waiting patiently in the stinky waiting area for hours, and may or may not be explained to about avoiding further stones by hydrating and alkalinizing his urine.
I could've explained it to him, he was incredibly healthy and intelligent compared to the normal potato heads with 4 or 5 chronic diseases like I normally see, but I didn't have the time to look it up, becuase I had just been served up a new patient by CHIEF RESIDENT, and so I gave him some Vicodin, and good luck. I just hope the next Eager New Doctor will have an attending who will go over the previous visit, and give him the explanation he deserves.
Now, simultaneously feeling I let CHIEF RESIDENT down by not seeing enough patients, and upset with him for subjecting my "private" patient to the indignity of an ambulatory walking fire hose up his penis, while his outpatient clinic urology appointment evaporates, and not getting the !@#$!#% CT abdo that I should have gotten during his first visit, I remember that he has two kids to take care of, and a life outside of medicine--he's human. I think, well, maybe he can't be my idol anymore, but that's okay. I'll just listen to my gut more.
The last two shifts, I humped hard, spurred by CHIEF RESIDENT's admonition that interns should see 10-12 patients per 12-hour shift. I was already working as hard as I could, I thought. Much of my time was spend figuring out how things were done, like how you have to order oral contrast separately if you order a gut CT, or worse, how I am still mystified by the computer's admission procedure, wasting my precious minutes and those of residents asking for help. I console myself, thinking, well, you'll learn to run those computer gears until they hum. I console myself, because I know eventually pressure for THROUGHPUT will eat away at time I use consoling, explaining, and cajoling patients into, through, and and after their ED visits.
I think of the time that I didn't take explaining to a kindly 61 year old postman, who I had seen 2 shifts earlier in the ER, returning with the same problem, urinary retention (which I ultimately discovered was due to not BPH or some horrible abdominal pathology, but just a stupid stone), now with an uncomfortable leg bag an indwelling foley penis catheter, placed by my idol, CHIEF RESIDENT, in a misguided attempt to avoid uremia, while not getting the test that would have simplified everything, a CT abdo) and his darling, caring wife, about his uric acid kidney stones and how to avoid them, because that's for his primary medical doctor, isn't it? Only, this couple is new to the medical game and is UNCLEAR ON THE CONCEPT of private physicians for people with good insurance, and gov't insurance is superb. So he will go to whatever shmuck intern will see him in the clinic, waiting patiently in the stinky waiting area for hours, and may or may not be explained to about avoiding further stones by hydrating and alkalinizing his urine.
I could've explained it to him, he was incredibly healthy and intelligent compared to the normal potato heads with 4 or 5 chronic diseases like I normally see, but I didn't have the time to look it up, becuase I had just been served up a new patient by CHIEF RESIDENT, and so I gave him some Vicodin, and good luck. I just hope the next Eager New Doctor will have an attending who will go over the previous visit, and give him the explanation he deserves.
Now, simultaneously feeling I let CHIEF RESIDENT down by not seeing enough patients, and upset with him for subjecting my "private" patient to the indignity of an ambulatory walking fire hose up his penis, while his outpatient clinic urology appointment evaporates, and not getting the !@#$!#% CT abdo that I should have gotten during his first visit, I remember that he has two kids to take care of, and a life outside of medicine--he's human. I think, well, maybe he can't be my idol anymore, but that's okay. I'll just listen to my gut more.
Dr. DeAngleis, JAMA Ed-in-chief
Cross-posted from Kevin's post about JAMA's "No Free Lunch" editor-in-chief
My prediction: Dr. DeAngleis will be good for JAMA, and for the AMA. Our top journals being direct to doctor advertisement has got to stop, or at least be recognized.
Why? Because trust is an issue. People's trust in doctors, hand-patters nonwithstanding, depends on their judgement. A doctor acts as a judge in medical matters, weighing evidence and coming to a ruling regarding the perpetrator and the treatment. What if we allowed real judges to accept money from the prison-industrial complex, or even influence in the form of studies that showed that perps who go through CCA's or Wackenhut's "rehabilitation" end up being model citizens? Or what if we did an end run and allowed these co's to influence lawmakers (no, no, no, not in our fair country...) to mandate prison sentences, effectively tying judges' hands (since guilt is determined by juries in criminal, and, dare I say it, medical malpractice cases) by removing judicial (and by allegorical extension, doctors') discretion?
Don't think it hasn't happened to medicine. Quick, what is standard of care for hyperlipidemia? Depression? Non-resectable breast cancer? Hypertension? Urinary retention? Alzheimer's? Upper respiratory tract infection? Come ON! These medical standards were defined by ghost written articles in top journals, subsequently flogged by drug reps over free eggplant parmesean, and finally begged for by patients after watching Bob Dole waltz his way into Viagra-enabled ecstasy.
In addition, medical journals, which target a very small and relatively wealthy population, often restrict advertising (NEJM) to pharmaceutical companies and drug-device manufacturers. Thus, the existence and publication of the journal itself depends on drug advertising. Going back to our metaphor, how would you like to see a leading criminal law journal restrict its advertising to CCA and Wackenhut?
My prediction: Dr. DeAngleis will be good for JAMA, and for the AMA. Our top journals being direct to doctor advertisement has got to stop, or at least be recognized.
Why? Because trust is an issue. People's trust in doctors, hand-patters nonwithstanding, depends on their judgement. A doctor acts as a judge in medical matters, weighing evidence and coming to a ruling regarding the perpetrator and the treatment. What if we allowed real judges to accept money from the prison-industrial complex, or even influence in the form of studies that showed that perps who go through CCA's or Wackenhut's "rehabilitation" end up being model citizens? Or what if we did an end run and allowed these co's to influence lawmakers (no, no, no, not in our fair country...) to mandate prison sentences, effectively tying judges' hands (since guilt is determined by juries in criminal, and, dare I say it, medical malpractice cases) by removing judicial (and by allegorical extension, doctors') discretion?
Don't think it hasn't happened to medicine. Quick, what is standard of care for hyperlipidemia? Depression? Non-resectable breast cancer? Hypertension? Urinary retention? Alzheimer's? Upper respiratory tract infection? Come ON! These medical standards were defined by ghost written articles in top journals, subsequently flogged by drug reps over free eggplant parmesean, and finally begged for by patients after watching Bob Dole waltz his way into Viagra-enabled ecstasy.
In addition, medical journals, which target a very small and relatively wealthy population, often restrict advertising (NEJM) to pharmaceutical companies and drug-device manufacturers. Thus, the existence and publication of the journal itself depends on drug advertising. Going back to our metaphor, how would you like to see a leading criminal law journal restrict its advertising to CCA and Wackenhut?
Wednesday, August 02, 2006
Doctor Nirvana

Ahh, I'm there.
Doctor Nirvana.
Cheerfully and expertly spouting nearly-useless facts while taking 6 hours to clean a miniscule big toe lac and close it with Steri Strips. Why did it take so long, do you ask?
Because I have to ask permission to wipe my ass.
Okay, I've bundled up two lacs in a row (because I must fill in THE CREDENTIALLING LOG with lacs and pelvics and nose tamponades and arterial punctures and foley catheterizations) and while the first one is dealt with (it takes twice as long to do the paperwork as it does to care for the patient--by the end of the year I hope to be spending only the same amount of time doing paperwork as doing patient care (one of the reasons why I like EM is that a progress note can consist of "Surgery admitted the patient, then the CT came back normal, then surgery signed off; discharge (ahh, the triple parenthetical. Now I've reached blogging, or as I prefer to call it blooging, nirvana))) the second lies down on the gurney, and I clean off his lac with gushes and high-pressure streams of saline (the solution to pollution is dilution), while discoursing learnedly on how hydrogen peroxide is useless as a wound cleaner, because all it does is react with the peroxidase in RBC's, killing them and releasing O2, while simultaneously lysing clots, which knit a wound together, but is marvelous as a cleaner of old dried blood. Ahh, tis a fine line between a run-on sentence and a complex predicate with several dependent clause, and the semicolon is your best friend. Doo-be-doo-wah! Yeah! Yeah! Yeah!
And the patient lies there(dang, can't start a sentence with a conjunction! Damage control!), with his 18 year old muscle bound brother who's going to law school, even though he's 18 and must only just be entering college, with a "Trust me I'm a lawyer" t-shirt, in a marvelous (oops, can't use the same adjective twice in such proximity, try the thesaurus--ahh, exemplary display of inner-city irony and po-mo-ism, as I regale him with medical minutiae, gently and with laughter, not tears, steering him away from the camp of the sodomites; I find a fairly superficial scratch that managed to penetrate his calluses. Problem? A scratch. Solution? Go home, weenie! Oh, no. Not so fast, buster. First you must clear it with the ATTENDING. Because it's their ass with the malpractice insurance, and my ass that will be chewed if I maange a patient without their holding my hand, because after all, I'm just an intern, and really know just about zip about anything. But before all of this happened, CHIEF RESIDENT had to come in and demonstrate the REGIONAL NERVE BLOCK, which, I have to admit, was kind of cool, (how long can this paragraph go on? Keep reading and find out!) however useless (as the pt went home with steri-strips, and not sutures, cf. above), and the SECOND YEAR RESIDENT (i.e. REAL resident, as opposed to me, a FAKE resident, because while it says RESIDENT on my badge, I'm really just an INTERN, and therefore, know knothing and must. have. hand. held.) comes in and inquires about the undermined CALLUS on said big toe which is sure to come off at some point in the future, when the wound may require RE-EVALUATION by yet some other, higher authority in the hierarchy, to ensure cosmesis (great word, used almost exclusively in ER, for "a good cosmetic result," meaning, dem wound edges, dey be apposed, and yet miraculously NOT UNDER TENSION! by the surgical ties, i.e. sutures, that bind them), when the ATTENDING finally, later comes in, takes one look, and says--hmm. superficial. Wound edges apposed. d/c. ON KEFLEX (a powerful antibiotic used for COMPLICATED! skin infections (which this decidedly was not, being a SCRATCH), and OH GOD! OHMIGOD DID YOU MAKE SURE HE HAS TETANUS PROPHYLAXIS? Did you ask five times? Did you give it anyway?
That's why it took six hours to treat a scrach under some poor schlub's big toe.

Ahh, I'm there.
Doctor Nirvana.
Cheerfully and expertly spouting nearly-useless facts while taking 6 hours to clean a miniscule big toe lac and close it with Steri Strips. Why did it take so long, do you ask?
Because I have to ask permission to wipe my ass.
Okay, I've bundled up two lacs in a row (because I must fill in THE CREDENTIALLING LOG with lacs and pelvics and nose tamponades and arterial punctures and foley catheterizations) and while the first one is dealt with (it takes twice as long to do the paperwork as it does to care for the patient--by the end of the year I hope to be spending only the same amount of time doing paperwork as doing patient care (one of the reasons why I like EM is that a progress note can consist of "Surgery admitted the patient, then the CT came back normal, then surgery signed off; discharge (ahh, the triple parenthetical. Now I've reached blogging, or as I prefer to call it blooging, nirvana))) the second lies down on the gurney, and I clean off his lac with gushes and high-pressure streams of saline (the solution to pollution is dilution), while discoursing learnedly on how hydrogen peroxide is useless as a wound cleaner, because all it does is react with the peroxidase in RBC's, killing them and releasing O2, while simultaneously lysing clots, which knit a wound together, but is marvelous as a cleaner of old dried blood. Ahh, tis a fine line between a run-on sentence and a complex predicate with several dependent clause, and the semicolon is your best friend. Doo-be-doo-wah! Yeah! Yeah! Yeah!
And the patient lies there(dang, can't start a sentence with a conjunction! Damage control!), with his 18 year old muscle bound brother who's going to law school, even though he's 18 and must only just be entering college, with a "Trust me I'm a lawyer" t-shirt, in a marvelous (oops, can't use the same adjective twice in such proximity, try the thesaurus--ahh, exemplary display of inner-city irony and po-mo-ism, as I regale him with medical minutiae, gently and with laughter, not tears, steering him away from the camp of the sodomites; I find a fairly superficial scratch that managed to penetrate his calluses. Problem? A scratch. Solution? Go home, weenie! Oh, no. Not so fast, buster. First you must clear it with the ATTENDING. Because it's their ass with the malpractice insurance, and my ass that will be chewed if I maange a patient without their holding my hand, because after all, I'm just an intern, and really know just about zip about anything. But before all of this happened, CHIEF RESIDENT had to come in and demonstrate the REGIONAL NERVE BLOCK, which, I have to admit, was kind of cool, (how long can this paragraph go on? Keep reading and find out!) however useless (as the pt went home with steri-strips, and not sutures, cf. above), and the SECOND YEAR RESIDENT (i.e. REAL resident, as opposed to me, a FAKE resident, because while it says RESIDENT on my badge, I'm really just an INTERN, and therefore, know knothing and must. have. hand. held.) comes in and inquires about the undermined CALLUS on said big toe which is sure to come off at some point in the future, when the wound may require RE-EVALUATION by yet some other, higher authority in the hierarchy, to ensure cosmesis (great word, used almost exclusively in ER, for "a good cosmetic result," meaning, dem wound edges, dey be apposed, and yet miraculously NOT UNDER TENSION! by the surgical ties, i.e. sutures, that bind them), when the ATTENDING finally, later comes in, takes one look, and says--hmm. superficial. Wound edges apposed. d/c. ON KEFLEX (a powerful antibiotic used for COMPLICATED! skin infections (which this decidedly was not, being a SCRATCH), and OH GOD! OHMIGOD DID YOU MAKE SURE HE HAS TETANUS PROPHYLAXIS? Did you ask five times? Did you give it anyway?
That's why it took six hours to treat a scrach under some poor schlub's big toe.
