A Budding Emergencist
Friday, September 29, 2006
Tics!
My uncle recently had an interesting case of gut trouble. My uncle is a citizen of Spain, and presented there with bowel obstruction. Details are sketchy, but somehow my young (49), vigorous, unmedicated, chain-smoking, life-loving firecracker of an uncle ended up with an diverting colostomy.
Holy Cow!
What?
I thought he was gonna live forever!
My odious grandfather was the sick one! My uncle is one of us! Young, healthy, oppressed!
Recently, my odious grandfather passed away, leaving the sick role open for anyone to take up.
My aunt tried to take up the sick role with her divorce and depression, but her essential youth, responsibilities as a mother, and my family's circling of the wagons bouyed her, and now she's fine.
My grandmother, despite two hip replacements and age well over 80, is too interested in living to sacrifice herself to being sick.
My father, the eldest child, is simply too busy, with too many responsibilities (including, until recently, me, now gainfully employed).
That really left my other uncle, also a physician like my father and battling ankylosing spondylitis, yet with small children to raise. His time will come.
My uncle, the jolly travel agent, was next. His entry into the healthcare system was abrupt, severe, and expensive.
So after his colostomy, my father, an oncologist, arranged to have him fly to the States for the best medical care money can buy, at one of the nationally known best cancer centers in the U.S. (Hint: Not Sloan-Kettering), for surgical treatment of his supposed colon CA.
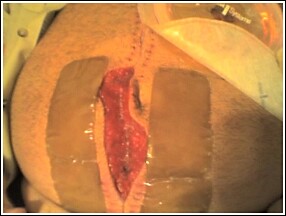
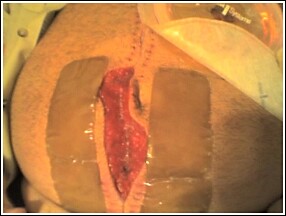
He got a private room and lots of amenities that impressed my father's family. His course was complicated by a laparotomy wound infection that left my uncle's wound to close by delayed primary closure.
Preop CT showed a thickening of the wall and constriction of a 10 cm length of ascending colon. Not exactly an apple core lesion, but good enough to resect. My father, the oncologist was concerned about cancer, but the lesion had not revealed itself on colonoscopy. I brought up the possibility of colitis and was ignored.
Grossly, the 10-cm section of colon in question showed diverticulitis and concomitant colitis. THe surgeon did not appreciate any cancerous mass, but the final pathology report is still pending. Meanwhile, my uncle experienced a surgical site infection that required removal of his sutures, allowing the pus to drain. Now he has a 15 x 8 open surgical wound, is afebrile and recovering, but still with colostomy.
My father wants to know about VAC dressing. At first I thought, "Is he on antibiotics? Why is he out of the hospital?" Then I remembered an old dictum from graduate school, "If you have a question, go to the library and look it up." Here's what I found:
"Vacuum Assisted Closure®
Fascial Vacuum Assisted Closure® (V.A.C.®) therapy (Kinetic Concepts, Inc, San Antonio, Tex) is a relatively new concept in the management of the open abdomen that allows for fascial closure as long as 1 month after the initial laparotomy. This avoids the need and attendant operative risks incurred with abdominal wall reconstruction in the future.
The main functional component of V.A.C.® is the use of a nonadherent, polyethylene sheet to cover the exposed viscera and the placement of a polyurethane sponge under controlled negative pressure. The polyethylene sheet helps prevent visceral-abdominal wall adhesions that inhibit movement of the abdominal wall. The polyurethane sponge, when placed under negative pressure (suction), provides the countertraction required to inhibit abdominal wall retraction" [ed note: (i.e. "loss of domain," when the abdominal cavity contracts after full or partial evisceration (in Pepe's case, an open (albeit with closed fascia from Alex's picture) laparotomy scar); if the wound was closed, the resultant increased pressure (because of decreased (contracted) abdominal volume) would create an abdominal compartment syndrome, decreasing blood flow to the kidney and mesenteric vessels. ) "and creates an environment where approximation of the abdominal wall may occur. The alternative is secondary (i.e. by myofibril contraction in the third phase of healing) healing, leaving a large scar after a prolonged (months) natural wound closure time, or delayed primary closure, possibly leading to skin grafts or subsequent infection."
However, this seems moot given the ileostomy in the picture--he's going to have to be opened up again in the near future to reanastamose the bowel. But, the vac may assist in a shorter delayed primary closure in the subsequent laparotomies as well, given the reduced loss of domain. By the way, I hope this episode has impressed upon [uncle] to improve his lifestyle re: smoking, obesity, and sedentary lifestyle...
Bonus: Surgical site infections patient risk factors:
Risk factors:
Systemic factors include age, malnutrition, hypovolemia, poor tissue perfusion, obesity, diabetes, steroids, and other immunosuppressants. Also smoking.
Wound characteristics include nonviable tissue in wound; hematoma; foreign material, including drains and sutures; dead space; poor skin preparation, including shaving; and preexistent sepsis (local or distant).
Operative characteristics include poor surgical technique; lengthy operation (>2 h); intraoperative contamination, including infected theater staff and instruments and inadequate theater ventilation; prolonged preoperative stay in the hospital; and hypothermia.
All from diverticulitis (tics!)
-the emergencist
P.S. Yeah, I know this post's not technically EM, but "wound healing, revisited" is. Has implications for trauma, too. So there.
My uncle recently had an interesting case of gut trouble. My uncle is a citizen of Spain, and presented there with bowel obstruction. Details are sketchy, but somehow my young (49), vigorous, unmedicated, chain-smoking, life-loving firecracker of an uncle ended up with an diverting colostomy.
Holy Cow!
What?
I thought he was gonna live forever!
My odious grandfather was the sick one! My uncle is one of us! Young, healthy, oppressed!
Recently, my odious grandfather passed away, leaving the sick role open for anyone to take up.
My aunt tried to take up the sick role with her divorce and depression, but her essential youth, responsibilities as a mother, and my family's circling of the wagons bouyed her, and now she's fine.
My grandmother, despite two hip replacements and age well over 80, is too interested in living to sacrifice herself to being sick.
My father, the eldest child, is simply too busy, with too many responsibilities (including, until recently, me, now gainfully employed).
That really left my other uncle, also a physician like my father and battling ankylosing spondylitis, yet with small children to raise. His time will come.
My uncle, the jolly travel agent, was next. His entry into the healthcare system was abrupt, severe, and expensive.
So after his colostomy, my father, an oncologist, arranged to have him fly to the States for the best medical care money can buy, at one of the nationally known best cancer centers in the U.S. (Hint: Not Sloan-Kettering), for surgical treatment of his supposed colon CA.
He got a private room and lots of amenities that impressed my father's family. His course was complicated by a laparotomy wound infection that left my uncle's wound to close by delayed primary closure.
Preop CT showed a thickening of the wall and constriction of a 10 cm length of ascending colon. Not exactly an apple core lesion, but good enough to resect. My father, the oncologist was concerned about cancer, but the lesion had not revealed itself on colonoscopy. I brought up the possibility of colitis and was ignored.
Grossly, the 10-cm section of colon in question showed diverticulitis and concomitant colitis. THe surgeon did not appreciate any cancerous mass, but the final pathology report is still pending. Meanwhile, my uncle experienced a surgical site infection that required removal of his sutures, allowing the pus to drain. Now he has a 15 x 8 open surgical wound, is afebrile and recovering, but still with colostomy.
My father wants to know about VAC dressing. At first I thought, "Is he on antibiotics? Why is he out of the hospital?" Then I remembered an old dictum from graduate school, "If you have a question, go to the library and look it up." Here's what I found:
"Vacuum Assisted Closure®
Fascial Vacuum Assisted Closure® (V.A.C.®) therapy (Kinetic Concepts, Inc, San Antonio, Tex) is a relatively new concept in the management of the open abdomen that allows for fascial closure as long as 1 month after the initial laparotomy. This avoids the need and attendant operative risks incurred with abdominal wall reconstruction in the future.
The main functional component of V.A.C.® is the use of a nonadherent, polyethylene sheet to cover the exposed viscera and the placement of a polyurethane sponge under controlled negative pressure. The polyethylene sheet helps prevent visceral-abdominal wall adhesions that inhibit movement of the abdominal wall. The polyurethane sponge, when placed under negative pressure (suction), provides the countertraction required to inhibit abdominal wall retraction" [ed note: (i.e. "loss of domain," when the abdominal cavity contracts after full or partial evisceration (in Pepe's case, an open (albeit with closed fascia from Alex's picture) laparotomy scar); if the wound was closed, the resultant increased pressure (because of decreased (contracted) abdominal volume) would create an abdominal compartment syndrome, decreasing blood flow to the kidney and mesenteric vessels. ) "and creates an environment where approximation of the abdominal wall may occur. The alternative is secondary (i.e. by myofibril contraction in the third phase of healing) healing, leaving a large scar after a prolonged (months) natural wound closure time, or delayed primary closure, possibly leading to skin grafts or subsequent infection."
However, this seems moot given the ileostomy in the picture--he's going to have to be opened up again in the near future to reanastamose the bowel. But, the vac may assist in a shorter delayed primary closure in the subsequent laparotomies as well, given the reduced loss of domain. By the way, I hope this episode has impressed upon [uncle] to improve his lifestyle re: smoking, obesity, and sedentary lifestyle...
Bonus: Surgical site infections patient risk factors:
Risk factors:
Systemic factors include age, malnutrition, hypovolemia, poor tissue perfusion, obesity, diabetes, steroids, and other immunosuppressants. Also smoking.
Wound characteristics include nonviable tissue in wound; hematoma; foreign material, including drains and sutures; dead space; poor skin preparation, including shaving; and preexistent sepsis (local or distant).
Operative characteristics include poor surgical technique; lengthy operation (>2 h); intraoperative contamination, including infected theater staff and instruments and inadequate theater ventilation; prolonged preoperative stay in the hospital; and hypothermia.
All from diverticulitis (tics!)
-the emergencist
P.S. Yeah, I know this post's not technically EM, but "wound healing, revisited" is. Has implications for trauma, too. So there.
Sunday, September 24, 2006
Physician Assistants
In response to some emails and some posts regarding my overbroad criticism of neuro PA's, I wrote the following email:
So, to all you PAs, please accept this olive branch.
I would just like to add that I did not start any fires at the time, either during the case or in the patient record. In the anonymity of this blog, however, I'll say what I think.
I appreciate the time you took to send a note-- As well, I am grateful you took the time to read my post.
I hope you will understand my consternation at the situation I was in. Here I was, watching as the fabric of medicine fell apart. I am not entirely sure (I didn't bring it up with that particular PA) but I think a goof was made. Whether it was made by the ER doc, the neurosurgeon, anaesthesia (who I point the biggest finger at, since that was the rotation I was in--anaesthesia is meant (from my understanding) to be a kind of "medical" check to surgery's go-go-cut mentality--i.e. gee the patient should have adequate attention paid to his coagulation status before surgery.), or the neurosurgery PA, the patient is the one who suffered. In defense of anaesthesia, the case was done "emergently," meaning rapid sequence intubation, and then please STFU, anaesthesia.
My understanding of the position of the PA in this is full of holes. I do not know how much responsibility they have. I know that my father employs NPs to great effect as "physician extenders"--i.e. they are equipped to make medical decisions and act basically at the level of a mid-level resident. Is this wrong? I know that my hospital employs many PAs in the ED for nonacute cases, SIGNIFICANTLY (via "fasttrack" etc.) improving the situation for both ER docs and patients. My dad loves his NPs because he doesn't have to worry that's they're doing some crazy shit and not telling him, like some doctors that he's previously employed (and subsequently fired). NPs (and by extension PAs) are the perfect solution to this problem of the doctor (in my fathers' case, an oncologist in a rural area) not being physically able to see all the patients. Given enough information from a trusted source, management can be effected, often with brilliant results, by a physician extender, in the same way that a decent resident (i.e. me) can enable a primary care doc to see maybe not twice as many patients, but maybe 1.5 times as many. Bullshit like documentation can be comfortably delegated to an experienced practitioner. At LAC+USC, where I bowed before the gods of EM, PAs who had been there 20+ years taught the residents casting, splinting, and suturing. Again, brilliant.
HOWEVER. In this case, and with this particular PA, I feel he overstepped his bounds, failing to adequately ensure coagulation balance before the first surgery, which would have prevented the second surgery. Of course, if the first surgery was also emergent, then this whole episode falls under the category of "the patient had a complication because the patient was sick." This is partly the fault of the neurosurgeon. This particular PA has also berated and abused my senior attending anesthesiologist (with 20+ years experience in neuroanesthesia) for some bullshit I don't even give the credit of memory for. (extreme chutzpah). This mirrors the attitude of another neuro PA in a different hospital abusing medical students (namely me). So you'll forgive me if I've got a sore spot when it comes to neuro PAs. I've had very favorable encounters with PA's in other disciplines. I value the role that PAs play as long as they don't aggrandize themselves above other doctors they work with, to the extent of unprofessional behavior. It just stands out more---that which may be forgiven in an attending is certainly not excused in a PA--which illustrates the difficult nature of the job.
I have generally quite positive impressions of PAs and other "midlevel" practitioners, Dr. Crippen (NHS Blog) and his quacktitioner crusade notwithstanding. Midwives fill an absolutely critical role in my neighborhood, where I can count the number of OB-GYN's on both hands for a population of millions.
so, my hat's off to you, and sorry if I offended,
Yours,
Dex, the emergencist.
So, to all you PAs, please accept this olive branch.
I would just like to add that I did not start any fires at the time, either during the case or in the patient record. In the anonymity of this blog, however, I'll say what I think.
Thursday, September 14, 2006
Bad Reaction to Anaesthesia?

I page the attending anaesthesiologist.
"Hello, Dr. H? The patient is in the room."
"Already? Ok, fine."
At this point, I'd already seen the patient with the resident (the REAL resident, not me the fake resident. The morning lecturer had referenced a clarification about autotranfusion postpartum I had asked for after her previous week's OB gas lecture, noting that "the medical student" had made a good point. I'm still a little raw about it.) I'd already gone through the history, a s/p posterior cervical laminectomy for numbness/weakness/paresthesias in fingers and toes the day before. The resident and I had already "lined-up" the patient with EKG, 02 sat, BP cuff, 3L nasal cannula, and transferred him to the operating table. All was left was to paralyze him, intubate him, and position him to the neurosurgeons preference. An emergent surgery for acute epidural hematoma.
Curiously, the patient had also developed b/l DVTs between admission and , so for an unexplained reason they had already put a greenfield filter in--as medical management is the standard of care, however, perhaps they had already anticipated the current complication which contraindicates anticoagulation --epidural hematoma. However, the complication had already occurred? Why?
This line of questioning had lead me to investigate lab values--INR 1.3--a little high. Why? No coumadin on board. No record of heparinization. Also no LFTs. Ah.
My curiosity is piqued. How does a patient with an obvious bleeding diasthesis go for a week in the hosptial without liver function tests? I can only assume neurosurgical oversight. Reminds me of an old joke:
So anyway, I mention the probable liver disease in this 65 year old man. "Ah well," he says, "it doesn't matter anyway." "But won't it make the patient harder to wake up? I mean, we should reduce the dose of anesthesia." "Nah."
Not surprisingly to me, the patient took a full half hour to wake up and be extubated. I looked ruefully at the drainage bag from the posterior cervical incision site, draining almost 500cc of bright red blood (an indication of poor clotting, another indicator of severe liver disease) by the time we got to the recovery room.
This patient came in without a primary care doctor. I think this is the reason why he got such shoddy care ( = ignorance of liver function status.) If an intern in a normally hypervigilant and over-testing-prone teaching hospital can spot a failure of care, it's bad.
On the ER note of this respectable, employed, family-oriented grandfather?
"Alcohol use: 3+ drinks of hard liqour per day x 30 years."
Nobody reads the ER chart.
Sigh.
-The Emergencist
P.S. Yes I had a great time hyperlinking this post.

I page the attending anaesthesiologist.
"Hello, Dr. H? The patient is in the room."
"Already? Ok, fine."
At this point, I'd already seen the patient with the resident (the REAL resident, not me the fake resident. The morning lecturer had referenced a clarification about autotranfusion postpartum I had asked for after her previous week's OB gas lecture, noting that "the medical student" had made a good point. I'm still a little raw about it.) I'd already gone through the history, a s/p posterior cervical laminectomy for numbness/weakness/paresthesias in fingers and toes the day before. The resident and I had already "lined-up" the patient with EKG, 02 sat, BP cuff, 3L nasal cannula, and transferred him to the operating table. All was left was to paralyze him, intubate him, and position him to the neurosurgeons preference. An emergent surgery for acute epidural hematoma.
Curiously, the patient had also developed b/l DVTs between admission and , so for an unexplained reason they had already put a greenfield filter in--as medical management is the standard of care, however, perhaps they had already anticipated the current complication which contraindicates anticoagulation --epidural hematoma. However, the complication had already occurred? Why?
This line of questioning had lead me to investigate lab values--INR 1.3--a little high. Why? No coumadin on board. No record of heparinization. Also no LFTs. Ah.
My curiosity is piqued. How does a patient with an obvious bleeding diasthesis go for a week in the hosptial without liver function tests? I can only assume neurosurgical oversight. Reminds me of an old joke:
An intern and a crusty old attending were rounding the corner to the elevator when the attending spied one going their way. Moving with a speed heretofore unsuspected by the intern, the attending just manages to wedge his hand in between the elevator door and the jamb, whereupon it opens. The intern gasps, "Doctor! You could've lost a hand!" The salty old medicine attending replied with a shrug, "Well, I'm an internal medicine doctor. I don't really need my hands anyway!" The intern ponders this significantly as the doors begin to close again. The intern glances up and sees a surgical resident dashing towards the elevator door. Just as the door is closing, the surgical resident sticks his head in between the closing door and the jamb.
So anyway, I mention the probable liver disease in this 65 year old man. "Ah well," he says, "it doesn't matter anyway." "But won't it make the patient harder to wake up? I mean, we should reduce the dose of anesthesia." "Nah."
Not surprisingly to me, the patient took a full half hour to wake up and be extubated. I looked ruefully at the drainage bag from the posterior cervical incision site, draining almost 500cc of bright red blood (an indication of poor clotting, another indicator of severe liver disease) by the time we got to the recovery room.
This patient came in without a primary care doctor. I think this is the reason why he got such shoddy care ( = ignorance of liver function status.) If an intern in a normally hypervigilant and over-testing-prone teaching hospital can spot a failure of care, it's bad.
On the ER note of this respectable, employed, family-oriented grandfather?
"Alcohol use: 3+ drinks of hard liqour per day x 30 years."
Nobody reads the ER chart.
Sigh.
-The Emergencist
P.S. Yes I had a great time hyperlinking this post.
Friday, September 08, 2006
Book Review or Practice Vision?
"Just trying to save a few lives: tales of life and death in the ER" by Pamela Grim, M.D. Warner, 2000.
As I move through my hospital's departments, everybody asks me what I'm going to be when I "grow up," a familiar refrain from medical school, only now I'm a doctor, being paid to repeat my 4th year. Can't complain. Right now I'm in anaesthesia, and this week's subject is scopes. Endoscopies and colonoscopies. Guts. Poop. As a future ER doc, I have superhuman powers--among them is emotional immunity to all bodily fluids. As wet, Golytely inspired farts escape around the colonoscope, which looks surprisingly like a bronchoscope, or the endoscope, the GI docs grimace and apologize to everybody in the room, for the noise, and the smell, which is considerable. Most of us are concentrating on our tasks, and a little smile comes to my face as I think, "you're gonna have to do better than that to gross me out." It's surprising that a GI doc would have such almost Victorian attitudes towards farting, especially since his job consists of inserting tubes in people's butts all day long.
So one unusually talkative GI doc asks me, de rigeur, what I'm going into, after similarly grilling and passing judgement on the medical student's hopes and dreams (anesthesia: approval!). His reaction to my choice, EM, is kind of a pained, confused look. His explanation of his disapproval is, "why would you want to be an intern for the rest of your life?" i.e., presenting patients to specialists.
His second criticism of ER is that, well, gee, you have to know so much! Yes, there are classic emergencies, bread and butter stuff, acute MI, stroke, sepsis...but what do you do if you don't know what to do and there is no specialist to save your butt? His example was a bad fracture of, say, a hand, where you have no plastic/hand surgeon to consult, for example in a rural ER.
I was amused. Mainly becuase, even in my limited 8+ weeks or so of direct ER experience, I'd already managed many open fractures of the hand, and started reciting the management, "well, you've got to explore the wound to assess integrity of the tendons and the joint capsules, and generally start antibiotics--I'm thinking ancef, here--and don't close, cuz they'll need to do washout and further inspection...oh wait." Hmm, no hand/plastics/ortho? What to do if no orthopod is around or willing to carry the ball after you stabilize? Do you turn the ER into some kind of half-assed clinic or make an appointment with any available specialist, knowing full well that, unlike in the ER, wallet biopsies will be performed as triage in those offices?
And so, on to the book review, and the darker world of a lone star ER doc. ER docs have a reputation for being "cowboys". In fact, it's one of the aspects of ER that attracted me initially when I did my first ER rotation as a student on the opposite coast in a huge County hospital. How few consults and non-ER specialists I saw! A closed ER, where anybody there is ER's responsibility! How many residents I saw routinely handling cases where specialists in my top-heavy home hospital would fear to tread!
They used to joke, after presenting cases for M & M, how all patients belong in "C-Booth!" corresponding to my current hospital's resuscitation room. The irony, of course being, that ER docs, especially at that hospital, would routinely and confidently manage complicated and decompensating patients that would make residents from other specialties croak in terror, making yellow stains all over their pristine white coats. Cowboys (and cowgirls!).
Dr. Grim illustrates the flip side of this aspect of ER: [spoilers ahead! Avast!] that, given an impossible situation where help is nowhere to be found, YOU are the doctor. The buck stops with you. If there is nobody to pass the ball off to, you're it. She does so with cases of precipitous deliveries in the ER, including several stillbirths, maternal deaths, and one eye-popping case of anencephaly. Also cases of frustration and death, sometimes of colleagues (police officers are considered comrades and brothers-in-arms of ER ppl). Stories of beating your head against the wall, trying desperately to put your finger in the dam of afflicted humanity swamping our nation's ERs. Walking wounded and the uninsured, punctuated by the occasional actual trauma or resuscitation. She talks of burnout.
The dreaded B-word, second only in potency to the dreaded C-word. I've heard tell that this happens much less often to board-certified and trained ER docs versus the "other" specialties grandfathered into ER work. The crux of the matter is this--since you are a cowboy, you must also undergo significantly more scrutiny, both from within and from without, of your management of cases you may or may not be qualified to handle. But you were there, and you were it. So you did your best. But the criticism doesn't care. Thus are born the seeds of destruction--self-doubt leading to burnout.
Other contributing factors include simply the sheer volume and magnitude of bad news that you are intimately involved with. Death, disability, and disfigurement--ER docs are often the first, and sometimes, only doctors to take responsibility for such cases. According to the books' phenomenology of burnout, you gradually lose contact with emotions and become numb as the emotional overload of suffering and stupidity and frustration, amortized over years, gradually strips you of your humanity. Personal insight is the first emotional capability to go--thus assuring your continued downward spiral if left unaddressed by coworkers, etc., since you are unaware of your ever-more-limited emotional and psychological coping mechanisms dissolving away. Eventually the only emotion left is anger, which quickly becomes your permanent and dominant emotion, subject to irrational outbursts and "small stuff," manifesting finally as burnout when the frayed nerves snap.
She also describes insane schedules that contribute to burnout, like "after the tenth/twelth 12-hour shift," which is a bright spot as this situation no longer exists as far as I know. Side note--I'm told by CHIEF RESIDENT that residents' hours are limited to 60 (versus 80 for floor schlubs) and that they are calculated week-to-week, starting Monday, at least at my institution, with no more than five days of shifts per 7-day period. When I asked him about the difference between these hours and other residents' hours, he said--it's because 60 hours in the ER is like 80 hours on the floor. My other rotating interns' experiences mirror mine in that you don't really get a chance to sit down or take a break for most if not all of those 12 hours.
Her descent is vivid and gripping, although blog-like and autobiographically pedestrian (I was struck with the similarities between some of her chapters and some blog entries I had read) at times. A philosophy professor in my sophomore year at college (Robert Goff, Ph.D. at UCSC), a textbook unto himself, regularly dispensed such pearls as , "Don't psychoanalyze your friends!" which I remember and continue to apply in my life. One of these, echoing Bob Dylan, "Behind everything beautiful there's some kind of pain," was that yes, beauty comes from pain, suffering, and anguish, but there's a difference between true craftsmanship and simply spiiling your guts out onto the page. I'm afraid Dr. Grim devolves into the latter at times, telling her best "war stories," without really integrating them meaningfully into her narrative. Other characters are flat, and the chapters are haphazardly arranged, jumping between time periods, linked only loosely by theme. One gets the sense of exploitatation of these patients' pain in the service of the doctor's effort to save herself, but we are not taken along for the ride. Still, a gripping account of the state of EM and healthcare in general in this country, linked together with a useful insight into the nature of burnout.
-The Emergencist.
"Just trying to save a few lives: tales of life and death in the ER" by Pamela Grim, M.D. Warner, 2000.
As I move through my hospital's departments, everybody asks me what I'm going to be when I "grow up," a familiar refrain from medical school, only now I'm a doctor, being paid to repeat my 4th year. Can't complain. Right now I'm in anaesthesia, and this week's subject is scopes. Endoscopies and colonoscopies. Guts. Poop. As a future ER doc, I have superhuman powers--among them is emotional immunity to all bodily fluids. As wet, Golytely inspired farts escape around the colonoscope, which looks surprisingly like a bronchoscope, or the endoscope, the GI docs grimace and apologize to everybody in the room, for the noise, and the smell, which is considerable. Most of us are concentrating on our tasks, and a little smile comes to my face as I think, "you're gonna have to do better than that to gross me out." It's surprising that a GI doc would have such almost Victorian attitudes towards farting, especially since his job consists of inserting tubes in people's butts all day long.
So one unusually talkative GI doc asks me, de rigeur, what I'm going into, after similarly grilling and passing judgement on the medical student's hopes and dreams (anesthesia: approval!). His reaction to my choice, EM, is kind of a pained, confused look. His explanation of his disapproval is, "why would you want to be an intern for the rest of your life?" i.e., presenting patients to specialists.
His second criticism of ER is that, well, gee, you have to know so much! Yes, there are classic emergencies, bread and butter stuff, acute MI, stroke, sepsis...but what do you do if you don't know what to do and there is no specialist to save your butt? His example was a bad fracture of, say, a hand, where you have no plastic/hand surgeon to consult, for example in a rural ER.
I was amused. Mainly becuase, even in my limited 8+ weeks or so of direct ER experience, I'd already managed many open fractures of the hand, and started reciting the management, "well, you've got to explore the wound to assess integrity of the tendons and the joint capsules, and generally start antibiotics--I'm thinking ancef, here--and don't close, cuz they'll need to do washout and further inspection...oh wait." Hmm, no hand/plastics/ortho? What to do if no orthopod is around or willing to carry the ball after you stabilize? Do you turn the ER into some kind of half-assed clinic or make an appointment with any available specialist, knowing full well that, unlike in the ER, wallet biopsies will be performed as triage in those offices?
And so, on to the book review, and the darker world of a lone star ER doc. ER docs have a reputation for being "cowboys". In fact, it's one of the aspects of ER that attracted me initially when I did my first ER rotation as a student on the opposite coast in a huge County hospital. How few consults and non-ER specialists I saw! A closed ER, where anybody there is ER's responsibility! How many residents I saw routinely handling cases where specialists in my top-heavy home hospital would fear to tread!
They used to joke, after presenting cases for M & M, how all patients belong in "C-Booth!" corresponding to my current hospital's resuscitation room. The irony, of course being, that ER docs, especially at that hospital, would routinely and confidently manage complicated and decompensating patients that would make residents from other specialties croak in terror, making yellow stains all over their pristine white coats. Cowboys (and cowgirls!).
Dr. Grim illustrates the flip side of this aspect of ER: [spoilers ahead! Avast!] that, given an impossible situation where help is nowhere to be found, YOU are the doctor. The buck stops with you. If there is nobody to pass the ball off to, you're it. She does so with cases of precipitous deliveries in the ER, including several stillbirths, maternal deaths, and one eye-popping case of anencephaly. Also cases of frustration and death, sometimes of colleagues (police officers are considered comrades and brothers-in-arms of ER ppl). Stories of beating your head against the wall, trying desperately to put your finger in the dam of afflicted humanity swamping our nation's ERs. Walking wounded and the uninsured, punctuated by the occasional actual trauma or resuscitation. She talks of burnout.
The dreaded B-word, second only in potency to the dreaded C-word. I've heard tell that this happens much less often to board-certified and trained ER docs versus the "other" specialties grandfathered into ER work. The crux of the matter is this--since you are a cowboy, you must also undergo significantly more scrutiny, both from within and from without, of your management of cases you may or may not be qualified to handle. But you were there, and you were it. So you did your best. But the criticism doesn't care. Thus are born the seeds of destruction--self-doubt leading to burnout.
Other contributing factors include simply the sheer volume and magnitude of bad news that you are intimately involved with. Death, disability, and disfigurement--ER docs are often the first, and sometimes, only doctors to take responsibility for such cases. According to the books' phenomenology of burnout, you gradually lose contact with emotions and become numb as the emotional overload of suffering and stupidity and frustration, amortized over years, gradually strips you of your humanity. Personal insight is the first emotional capability to go--thus assuring your continued downward spiral if left unaddressed by coworkers, etc., since you are unaware of your ever-more-limited emotional and psychological coping mechanisms dissolving away. Eventually the only emotion left is anger, which quickly becomes your permanent and dominant emotion, subject to irrational outbursts and "small stuff," manifesting finally as burnout when the frayed nerves snap.
She also describes insane schedules that contribute to burnout, like "after the tenth/twelth 12-hour shift," which is a bright spot as this situation no longer exists as far as I know. Side note--I'm told by CHIEF RESIDENT that residents' hours are limited to 60 (versus 80 for floor schlubs) and that they are calculated week-to-week, starting Monday, at least at my institution, with no more than five days of shifts per 7-day period. When I asked him about the difference between these hours and other residents' hours, he said--it's because 60 hours in the ER is like 80 hours on the floor. My other rotating interns' experiences mirror mine in that you don't really get a chance to sit down or take a break for most if not all of those 12 hours.
Her descent is vivid and gripping, although blog-like and autobiographically pedestrian (I was struck with the similarities between some of her chapters and some blog entries I had read) at times. A philosophy professor in my sophomore year at college (Robert Goff, Ph.D. at UCSC), a textbook unto himself, regularly dispensed such pearls as , "Don't psychoanalyze your friends!" which I remember and continue to apply in my life. One of these, echoing Bob Dylan, "Behind everything beautiful there's some kind of pain," was that yes, beauty comes from pain, suffering, and anguish, but there's a difference between true craftsmanship and simply spiiling your guts out onto the page. I'm afraid Dr. Grim devolves into the latter at times, telling her best "war stories," without really integrating them meaningfully into her narrative. Other characters are flat, and the chapters are haphazardly arranged, jumping between time periods, linked only loosely by theme. One gets the sense of exploitatation of these patients' pain in the service of the doctor's effort to save herself, but we are not taken along for the ride. Still, a gripping account of the state of EM and healthcare in general in this country, linked together with a useful insight into the nature of burnout.
-The Emergencist.
