Wednesday, August 30, 2006
Ahh, farewell ER (for now)
Ok, the stone has turned. My last ER shift has come and gone. It was a make-up shift, and it actually overlapped my Anaesthesia rotation by one day, so I missed orientation (wah.) Now I am in Anaesthesia (I prefer the English spelling), and generally enjoying it. My anaesthesia attending says that it is more important to know your anesthesiologist's credentials and understand what's involved in that aspect of a case as opposed to the surgeon, but after watching a CT surgeon do (surgere? surgerize?) a 6-hr, off-pump CABG on a 81-years-young patient, I'm not so sure. Both are important, I expect.
Seeing Sid Schwab and Scalpel as well as "old pal" platypus comment on my blog is nice. Thanks!
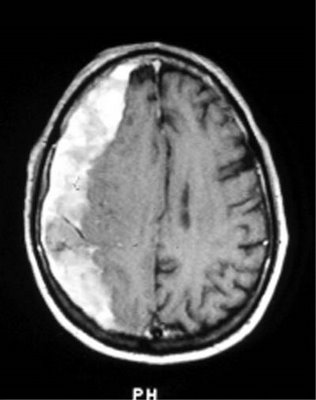
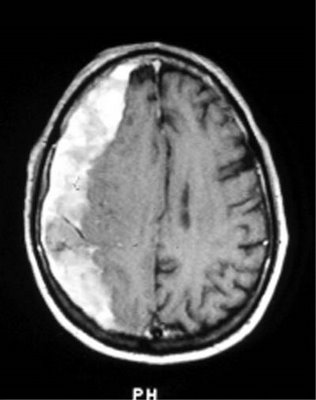
We had another VIP today at Metropolitan Medical Center, coming in for a 2 month old subacute subdural hematoma--a little out of the range (3 weeks) for subacute vs chronic, but that walked and talked like a subacute. Story goes, she (director of nursing for psychiatry, a nice lady and I trust her) was involved in a bad car wreck 2 months back, with her husband unfortunately receiving some pretty nasty lower extremity fractures. She got a nasty bump on her head along with some nausea/vomiting, and after the CT was read as normal, she was diagnosed with postconcussion syndrome. In the intervening two months, while her husband was being worked up for his fractures, she supported him while quietly cataloging and circular-filing her own symptoms, which included transient recurrent minor weakness in her left leg, transient numbness/tingling in her left arm, and an intruiging strip of paresthesia starting from the lateral canthus of her right eye and extending laterally into her scalp, not associated with tearing or dry eye. No N/V since then, no syncope, no cardiopulmonary symptoms, no seizures, no decreased level of consciousness.
[intermission: while these findings constitute focal neurologic signs, thus excluding PCS, I can imagine how, even in an experienced nurse, such a "diagnosis" can lead someone to minimize their symptoms until they become an impairment--"Oh, it's just my PCS acting up".]
[intermission #2: Nurses give great histories! This was like taking report on a patient instead of grinding out a history. VIP's are nice, for this and more reasons--they speak English, know their meds, know their history, and aren't afraid of mentioning things that other people would think the doctor "didn't need to know," like that bad reaction they had to penicillin 30 years ago resulting in an ICU stay, because medicine has really progressed since then, right?]
[there is NO intermission #3]
Being that the patient's regular doc was on vacation, she worked her grapevine to get expedited through the ER via my-favorite-attending, stopping by the CT and MRI machines for what she believed to be a transient ischemic attack, or mini-stroke. Well, she ended up fast-tracked to neurosurgery, where I saw her.
After a good deal of hand-patting, visits from our innumerable VP's and anxious relatives (uh, I mean, cowworker nurses), and a closed-session pep-talk by my anaestheia attending (who says anaesthesiologists don't talk to patients?), we got underway. After we had intubated and got some lines started, we waited around for the neurosurgeon awhile (sigh.). Finally the neurosurgery physician assistant comes in and immediately starts yelling! at my senior attending, for current and previous imagined slights! Agog, I stare unbelieving at this joker while he rants and whines about my attending for imagined slights (she wanted to talk to the surgeon about the case instead of this flunky) and finally leaves in a drama-queen huff. I mean, what is up with neurosurg PA's? They all seem to have a chip on their shoulder the size of Manhattan.
After the (rather young, given the 8-year residency neurosurgeon had come in and received his dose of abuse from the PA (while I again am shocked, chagrined, and stupefied at his impertinence. In the OR!), the surgery began. Nicely routine, with an interesting sidenote of how a subacute subdural will form a membrane around itself, leading to reformation of the hematoma despite every effort to prevent it. The surgeon explained that there is no way to prevent this, because stripping this extra membrane actually leads to increased recurrence of subdurals, and there is no way to "make the brain expand", like you would for a chronic pulmonary effusion to prevent recurrence. Long story short, the neurosurgeon started with Burr holes to evacuate the hematoma, and finding mainly solid hematoma, had to take out a chunk of skull to evacuate it, but otherwise the procedure went well, about 3 hours from the first cut.
After a teeth-grinding wait for transportation, I went and found a monitor myself after repeated overhead calls for a monitor (apparently VIP status doesn't faze the nursing attendants, of whom I've heard tell that if they stand up too fast they pass out. Trust an ER doc to do it himself. After that, our VIP went to recovery in the surgical intensive care unit, safe in the capable and caring hands of our SICU nurses.
Ok, the stone has turned. My last ER shift has come and gone. It was a make-up shift, and it actually overlapped my Anaesthesia rotation by one day, so I missed orientation (wah.) Now I am in Anaesthesia (I prefer the English spelling), and generally enjoying it. My anaesthesia attending says that it is more important to know your anesthesiologist's credentials and understand what's involved in that aspect of a case as opposed to the surgeon, but after watching a CT surgeon do (surgere? surgerize?) a 6-hr, off-pump CABG on a 81-years-young patient, I'm not so sure. Both are important, I expect.
Seeing Sid Schwab and Scalpel as well as "old pal" platypus comment on my blog is nice. Thanks!
We had another VIP today at Metropolitan Medical Center, coming in for a 2 month old subacute subdural hematoma--a little out of the range (3 weeks) for subacute vs chronic, but that walked and talked like a subacute. Story goes, she (director of nursing for psychiatry, a nice lady and I trust her) was involved in a bad car wreck 2 months back, with her husband unfortunately receiving some pretty nasty lower extremity fractures. She got a nasty bump on her head along with some nausea/vomiting, and after the CT was read as normal, she was diagnosed with postconcussion syndrome. In the intervening two months, while her husband was being worked up for his fractures, she supported him while quietly cataloging and circular-filing her own symptoms, which included transient recurrent minor weakness in her left leg, transient numbness/tingling in her left arm, and an intruiging strip of paresthesia starting from the lateral canthus of her right eye and extending laterally into her scalp, not associated with tearing or dry eye. No N/V since then, no syncope, no cardiopulmonary symptoms, no seizures, no decreased level of consciousness.
[intermission: while these findings constitute focal neurologic signs, thus excluding PCS, I can imagine how, even in an experienced nurse, such a "diagnosis" can lead someone to minimize their symptoms until they become an impairment--"Oh, it's just my PCS acting up".]
[intermission #2: Nurses give great histories! This was like taking report on a patient instead of grinding out a history. VIP's are nice, for this and more reasons--they speak English, know their meds, know their history, and aren't afraid of mentioning things that other people would think the doctor "didn't need to know," like that bad reaction they had to penicillin 30 years ago resulting in an ICU stay, because medicine has really progressed since then, right?]
[there is NO intermission #3]
Being that the patient's regular doc was on vacation, she worked her grapevine to get expedited through the ER via my-favorite-attending, stopping by the CT and MRI machines for what she believed to be a transient ischemic attack, or mini-stroke. Well, she ended up fast-tracked to neurosurgery, where I saw her.
After a good deal of hand-patting, visits from our innumerable VP's and anxious relatives (uh, I mean, cowworker nurses), and a closed-session pep-talk by my anaestheia attending (who says anaesthesiologists don't talk to patients?), we got underway. After we had intubated and got some lines started, we waited around for the neurosurgeon awhile (sigh.). Finally the neurosurgery physician assistant comes in and immediately starts yelling! at my senior attending, for current and previous imagined slights! Agog, I stare unbelieving at this joker while he rants and whines about my attending for imagined slights (she wanted to talk to the surgeon about the case instead of this flunky) and finally leaves in a drama-queen huff. I mean, what is up with neurosurg PA's? They all seem to have a chip on their shoulder the size of Manhattan.
After the (rather young, given the 8-year residency neurosurgeon had come in and received his dose of abuse from the PA (while I again am shocked, chagrined, and stupefied at his impertinence. In the OR!), the surgery began. Nicely routine, with an interesting sidenote of how a subacute subdural will form a membrane around itself, leading to reformation of the hematoma despite every effort to prevent it. The surgeon explained that there is no way to prevent this, because stripping this extra membrane actually leads to increased recurrence of subdurals, and there is no way to "make the brain expand", like you would for a chronic pulmonary effusion to prevent recurrence. Long story short, the neurosurgeon started with Burr holes to evacuate the hematoma, and finding mainly solid hematoma, had to take out a chunk of skull to evacuate it, but otherwise the procedure went well, about 3 hours from the first cut.
After a teeth-grinding wait for transportation, I went and found a monitor myself after repeated overhead calls for a monitor (apparently VIP status doesn't faze the nursing attendants, of whom I've heard tell that if they stand up too fast they pass out. Trust an ER doc to do it himself. After that, our VIP went to recovery in the surgical intensive care unit, safe in the capable and caring hands of our SICU nurses.
Comments:
<< Home
That reminded me of a similar patient I once saw in the ER. He was in his 60s if I recall correctly, and he used a bicycle for transportation after losing his driver's license from DWIs.
His complaint was that he was now too dizzy to ride his bicycle. On further questioning he told me that he had been hit in the head with a bat 3 months prior. He didn't have a headache.
His neuro examination in the stretcher was normal, but on standing he was quite unsteady and ataxic. His labs were normal, but his CT scan showed a huge chroonic subdural.
It's always good to get patients up and see how well they ambulate.
His complaint was that he was now too dizzy to ride his bicycle. On further questioning he told me that he had been hit in the head with a bat 3 months prior. He didn't have a headache.
His neuro examination in the stretcher was normal, but on standing he was quite unsteady and ataxic. His labs were normal, but his CT scan showed a huge chroonic subdural.
It's always good to get patients up and see how well they ambulate.
Verily. I appreciate your comments, Scalpel--do you want to be my blog attending? In my congested ER, walking about is contraindicated due to numerous workplace hazards even for health-care workers. So getting a patient up and ambulating is quite a trial. But the results are well worth it. All too often I see orthostasis, vertigo, cellulitis I didn't see before, a weak leg or legs, mental status changes, or pleasant LOLs in NAD without chief complaints who are too weak to walk--it is enough to justify walking every patient who can tolerate it every time. 4 steps is usually enough. And you can do a proper Romberg. Or convince an anxious family that granny is good to go home.
Safe, Low Priced MEN'S HEALTH Online!
Very Cheap Viagra, Levitra, Cialis, Lipitor, Propecia!
Buy Cheap Viagra Online
Free Prescription with your Order
The Lowest Prices Online
Complete PRIVACY
FedEx Overnight Shipping
Buy Viagra Online
Buy Online Propecia
Buy Lipitor Online
Buy Online Viagra
Buy Levitra Online
Buy Cialis Online
______
3 buy generic online viagra
buy online prescription propecia vaniqa viaga xenical
Buy Cialis Link Move Online
blogspot.com buy inurl online viagra
where to buy viagra online
buy cheap online viagra
2005 Buy Cialis January Online Period Summary
Very Cheap Viagra, Levitra, Cialis, Lipitor, Propecia!
Buy Cheap Viagra Online
Free Prescription with your Order
The Lowest Prices Online
Complete PRIVACY
FedEx Overnight Shipping
Buy Viagra Online
Buy Online Propecia
Buy Lipitor Online
Buy Online Viagra
Buy Levitra Online
Buy Cialis Online
______
3 buy generic online viagra
buy online prescription propecia vaniqa viaga xenical
Buy Cialis Link Move Online
blogspot.com buy inurl online viagra
where to buy viagra online
buy cheap online viagra
2005 Buy Cialis January Online Period Summary
Isenmesez
It's bad girl!
Niak sohk sabai jie te?
Ballpoint Book Guest Pen
Complete
Massage Therapist Dallas Tx
Florida Emergency Room Error Attorney
Carpet Cleaning Mildew
Back Pain Side
Cerebral Palsy Lawyer Philadelphia
Air Freight Carrier
Affiliate Progbram Sales
Concrete Balcony
Self Storage Facility Louisiana
Affiliawte Program Sales
Discount Storage Cabinet
Lift Weights
Aeronautical Science
Wrongful Death Lawyer Austin
Uz redzešanos
It's bad girl!
Niak sohk sabai jie te?
Ballpoint Book Guest Pen
Complete
Massage Therapist Dallas Tx
Florida Emergency Room Error Attorney
Carpet Cleaning Mildew
Back Pain Side
Cerebral Palsy Lawyer Philadelphia
Air Freight Carrier
Affiliate Progbram Sales
Concrete Balcony
Self Storage Facility Louisiana
Affiliawte Program Sales
Discount Storage Cabinet
Lift Weights
Aeronautical Science
Wrongful Death Lawyer Austin
Uz redzešanos
Gay Male Porn Star
Free Gay Military Porn Gay Man Porn Gay Teen Porn
Free Gay Porn Story Gay Porn Dvd Mature Gay Porn
Ebony Gay Porn Gay Guys Porn Gay Porn Trailer
Good Luck!
Post a Comment
Free Gay Military Porn Gay Man Porn Gay Teen Porn
Free Gay Porn Story Gay Porn Dvd Mature Gay Porn
Ebony Gay Porn Gay Guys Porn Gay Porn Trailer
Good Luck!
<< Home


