Friday, September 29, 2006
Tics!
My uncle recently had an interesting case of gut trouble. My uncle is a citizen of Spain, and presented there with bowel obstruction. Details are sketchy, but somehow my young (49), vigorous, unmedicated, chain-smoking, life-loving firecracker of an uncle ended up with an diverting colostomy.
Holy Cow!
What?
I thought he was gonna live forever!
My odious grandfather was the sick one! My uncle is one of us! Young, healthy, oppressed!
Recently, my odious grandfather passed away, leaving the sick role open for anyone to take up.
My aunt tried to take up the sick role with her divorce and depression, but her essential youth, responsibilities as a mother, and my family's circling of the wagons bouyed her, and now she's fine.
My grandmother, despite two hip replacements and age well over 80, is too interested in living to sacrifice herself to being sick.
My father, the eldest child, is simply too busy, with too many responsibilities (including, until recently, me, now gainfully employed).
That really left my other uncle, also a physician like my father and battling ankylosing spondylitis, yet with small children to raise. His time will come.
My uncle, the jolly travel agent, was next. His entry into the healthcare system was abrupt, severe, and expensive.
So after his colostomy, my father, an oncologist, arranged to have him fly to the States for the best medical care money can buy, at one of the nationally known best cancer centers in the U.S. (Hint: Not Sloan-Kettering), for surgical treatment of his supposed colon CA.
He got a private room and lots of amenities that impressed my father's family. His course was complicated by a laparotomy wound infection that left my uncle's wound to close by delayed primary closure.
Preop CT showed a thickening of the wall and constriction of a 10 cm length of ascending colon. Not exactly an apple core lesion, but good enough to resect. My father, the oncologist was concerned about cancer, but the lesion had not revealed itself on colonoscopy. I brought up the possibility of colitis and was ignored.
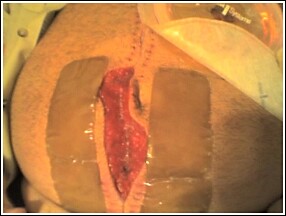
Grossly, the 10-cm section of colon in question showed diverticulitis and concomitant colitis. THe surgeon did not appreciate any cancerous mass, but the final pathology report is still pending. Meanwhile, my uncle experienced a surgical site infection that required removal of his sutures, allowing the pus to drain. Now he has a 15 x 8 open surgical wound, is afebrile and recovering, but still with colostomy.
My father wants to know about VAC dressing. At first I thought, "Is he on antibiotics? Why is he out of the hospital?" Then I remembered an old dictum from graduate school, "If you have a question, go to the library and look it up." Here's what I found:
"Vacuum Assisted Closure®
Fascial Vacuum Assisted Closure® (V.A.C.®) therapy (Kinetic Concepts, Inc, San Antonio, Tex) is a relatively new concept in the management of the open abdomen that allows for fascial closure as long as 1 month after the initial laparotomy. This avoids the need and attendant operative risks incurred with abdominal wall reconstruction in the future.
The main functional component of V.A.C.® is the use of a nonadherent, polyethylene sheet to cover the exposed viscera and the placement of a polyurethane sponge under controlled negative pressure. The polyethylene sheet helps prevent visceral-abdominal wall adhesions that inhibit movement of the abdominal wall. The polyurethane sponge, when placed under negative pressure (suction), provides the countertraction required to inhibit abdominal wall retraction" [ed note: (i.e. "loss of domain," when the abdominal cavity contracts after full or partial evisceration (in Pepe's case, an open (albeit with closed fascia from Alex's picture) laparotomy scar); if the wound was closed, the resultant increased pressure (because of decreased (contracted) abdominal volume) would create an abdominal compartment syndrome, decreasing blood flow to the kidney and mesenteric vessels. ) "and creates an environment where approximation of the abdominal wall may occur. The alternative is secondary (i.e. by myofibril contraction in the third phase of healing) healing, leaving a large scar after a prolonged (months) natural wound closure time, or delayed primary closure, possibly leading to skin grafts or subsequent infection."
However, this seems moot given the ileostomy in the picture--he's going to have to be opened up again in the near future to reanastamose the bowel. But, the vac may assist in a shorter delayed primary closure in the subsequent laparotomies as well, given the reduced loss of domain. By the way, I hope this episode has impressed upon [uncle] to improve his lifestyle re: smoking, obesity, and sedentary lifestyle...
Bonus: Surgical site infections patient risk factors:
Risk factors:
Systemic factors include age, malnutrition, hypovolemia, poor tissue perfusion, obesity, diabetes, steroids, and other immunosuppressants. Also smoking.
Wound characteristics include nonviable tissue in wound; hematoma; foreign material, including drains and sutures; dead space; poor skin preparation, including shaving; and preexistent sepsis (local or distant).
Operative characteristics include poor surgical technique; lengthy operation (>2 h); intraoperative contamination, including infected theater staff and instruments and inadequate theater ventilation; prolonged preoperative stay in the hospital; and hypothermia.
All from diverticulitis (tics!)
-the emergencist
P.S. Yeah, I know this post's not technically EM, but "wound healing, revisited" is. Has implications for trauma, too. So there.
My uncle recently had an interesting case of gut trouble. My uncle is a citizen of Spain, and presented there with bowel obstruction. Details are sketchy, but somehow my young (49), vigorous, unmedicated, chain-smoking, life-loving firecracker of an uncle ended up with an diverting colostomy.
Holy Cow!
What?
I thought he was gonna live forever!
My odious grandfather was the sick one! My uncle is one of us! Young, healthy, oppressed!
Recently, my odious grandfather passed away, leaving the sick role open for anyone to take up.
My aunt tried to take up the sick role with her divorce and depression, but her essential youth, responsibilities as a mother, and my family's circling of the wagons bouyed her, and now she's fine.
My grandmother, despite two hip replacements and age well over 80, is too interested in living to sacrifice herself to being sick.
My father, the eldest child, is simply too busy, with too many responsibilities (including, until recently, me, now gainfully employed).
That really left my other uncle, also a physician like my father and battling ankylosing spondylitis, yet with small children to raise. His time will come.
My uncle, the jolly travel agent, was next. His entry into the healthcare system was abrupt, severe, and expensive.
So after his colostomy, my father, an oncologist, arranged to have him fly to the States for the best medical care money can buy, at one of the nationally known best cancer centers in the U.S. (Hint: Not Sloan-Kettering), for surgical treatment of his supposed colon CA.
He got a private room and lots of amenities that impressed my father's family. His course was complicated by a laparotomy wound infection that left my uncle's wound to close by delayed primary closure.
Preop CT showed a thickening of the wall and constriction of a 10 cm length of ascending colon. Not exactly an apple core lesion, but good enough to resect. My father, the oncologist was concerned about cancer, but the lesion had not revealed itself on colonoscopy. I brought up the possibility of colitis and was ignored.
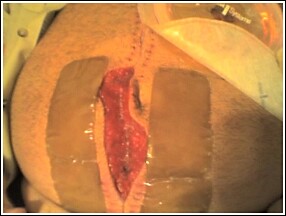
Grossly, the 10-cm section of colon in question showed diverticulitis and concomitant colitis. THe surgeon did not appreciate any cancerous mass, but the final pathology report is still pending. Meanwhile, my uncle experienced a surgical site infection that required removal of his sutures, allowing the pus to drain. Now he has a 15 x 8 open surgical wound, is afebrile and recovering, but still with colostomy.
My father wants to know about VAC dressing. At first I thought, "Is he on antibiotics? Why is he out of the hospital?" Then I remembered an old dictum from graduate school, "If you have a question, go to the library and look it up." Here's what I found:
"Vacuum Assisted Closure®
Fascial Vacuum Assisted Closure® (V.A.C.®) therapy (Kinetic Concepts, Inc, San Antonio, Tex) is a relatively new concept in the management of the open abdomen that allows for fascial closure as long as 1 month after the initial laparotomy. This avoids the need and attendant operative risks incurred with abdominal wall reconstruction in the future.
The main functional component of V.A.C.® is the use of a nonadherent, polyethylene sheet to cover the exposed viscera and the placement of a polyurethane sponge under controlled negative pressure. The polyethylene sheet helps prevent visceral-abdominal wall adhesions that inhibit movement of the abdominal wall. The polyurethane sponge, when placed under negative pressure (suction), provides the countertraction required to inhibit abdominal wall retraction" [ed note: (i.e. "loss of domain," when the abdominal cavity contracts after full or partial evisceration (in Pepe's case, an open (albeit with closed fascia from Alex's picture) laparotomy scar); if the wound was closed, the resultant increased pressure (because of decreased (contracted) abdominal volume) would create an abdominal compartment syndrome, decreasing blood flow to the kidney and mesenteric vessels. ) "and creates an environment where approximation of the abdominal wall may occur. The alternative is secondary (i.e. by myofibril contraction in the third phase of healing) healing, leaving a large scar after a prolonged (months) natural wound closure time, or delayed primary closure, possibly leading to skin grafts or subsequent infection."
However, this seems moot given the ileostomy in the picture--he's going to have to be opened up again in the near future to reanastamose the bowel. But, the vac may assist in a shorter delayed primary closure in the subsequent laparotomies as well, given the reduced loss of domain. By the way, I hope this episode has impressed upon [uncle] to improve his lifestyle re: smoking, obesity, and sedentary lifestyle...
Bonus: Surgical site infections patient risk factors:
Risk factors:
Systemic factors include age, malnutrition, hypovolemia, poor tissue perfusion, obesity, diabetes, steroids, and other immunosuppressants. Also smoking.
Wound characteristics include nonviable tissue in wound; hematoma; foreign material, including drains and sutures; dead space; poor skin preparation, including shaving; and preexistent sepsis (local or distant).
Operative characteristics include poor surgical technique; lengthy operation (>2 h); intraoperative contamination, including infected theater staff and instruments and inadequate theater ventilation; prolonged preoperative stay in the hospital; and hypothermia.
All from diverticulitis (tics!)
-the emergencist
P.S. Yeah, I know this post's not technically EM, but "wound healing, revisited" is. Has implications for trauma, too. So there.
Comments:
<< Home
Yikes, how shocking and difficult that must be for him. Best wishes for a quick recovery and negative pathology.
From an ED standpoint, it is interesting to me that the famous facility I think you refer to has an ED that only accepts their established cancer patients and their related emergencies. That would be an odd gig. One of my friends from residency works in that ED.
If your uncle doesn't actually have cancer and he is going to stay in this area, I know some outstanding surgeons in the Texas Medical Center that I would be happy to recommend.
From an ED standpoint, it is interesting to me that the famous facility I think you refer to has an ED that only accepts their established cancer patients and their related emergencies. That would be an odd gig. One of my friends from residency works in that ED.
If your uncle doesn't actually have cancer and he is going to stay in this area, I know some outstanding surgeons in the Texas Medical Center that I would be happy to recommend.
Thanks, scalpel--
I appreciate your offer very much--he is feeling better and on his way home to spain. Turned out to be colitis. That was my first thought, but hey! what do I know? That's right, intern. Nothing. Fine.
It would be interesting to work in an ER where all the presentations were cancer, cancer related, or in a patient who has/had cancer. I guess you would avoid the whole get-quiet-all-of-a-sudden, don't-tell-the-patient, treat-him-nice-he's-got-the-SEE-AAY!, type of treatment that newly diagnosed CA pts get at my hopsital.
Anyway.
Thanks again.
-Dex
Post a Comment
I appreciate your offer very much--he is feeling better and on his way home to spain. Turned out to be colitis. That was my first thought, but hey! what do I know? That's right, intern. Nothing. Fine.
It would be interesting to work in an ER where all the presentations were cancer, cancer related, or in a patient who has/had cancer. I guess you would avoid the whole get-quiet-all-of-a-sudden, don't-tell-the-patient, treat-him-nice-he's-got-the-SEE-AAY!, type of treatment that newly diagnosed CA pts get at my hopsital.
Anyway.
Thanks again.
-Dex
<< Home


